Myocarditis Mimicking ST-Elevation Myocardial Infarction: A Case Report
DOI:
https://doi.org/10.38179/ijcr.v4i1.198Keywords:
STEMI, Acute myocardial injury, Myocarditis, CMR, Case ReportAbstract
Background: Myocarditis is the inflammation of the heart muscle, which affects mostly the young population. Patients may experience symptoms ranging from chest pain, fatigue, dyspnea, to more serious conditions such as heart failure and arrhythmias. Diagnosis of myocarditis may be quite confusing as it may mimic myocardial infarction, particularly when ST-elevation is present on electrocardiogram (ECG). Here, we present a challenging presentation of myocarditis mimicking ST-segment elevation myocardial infarction (STEMI).
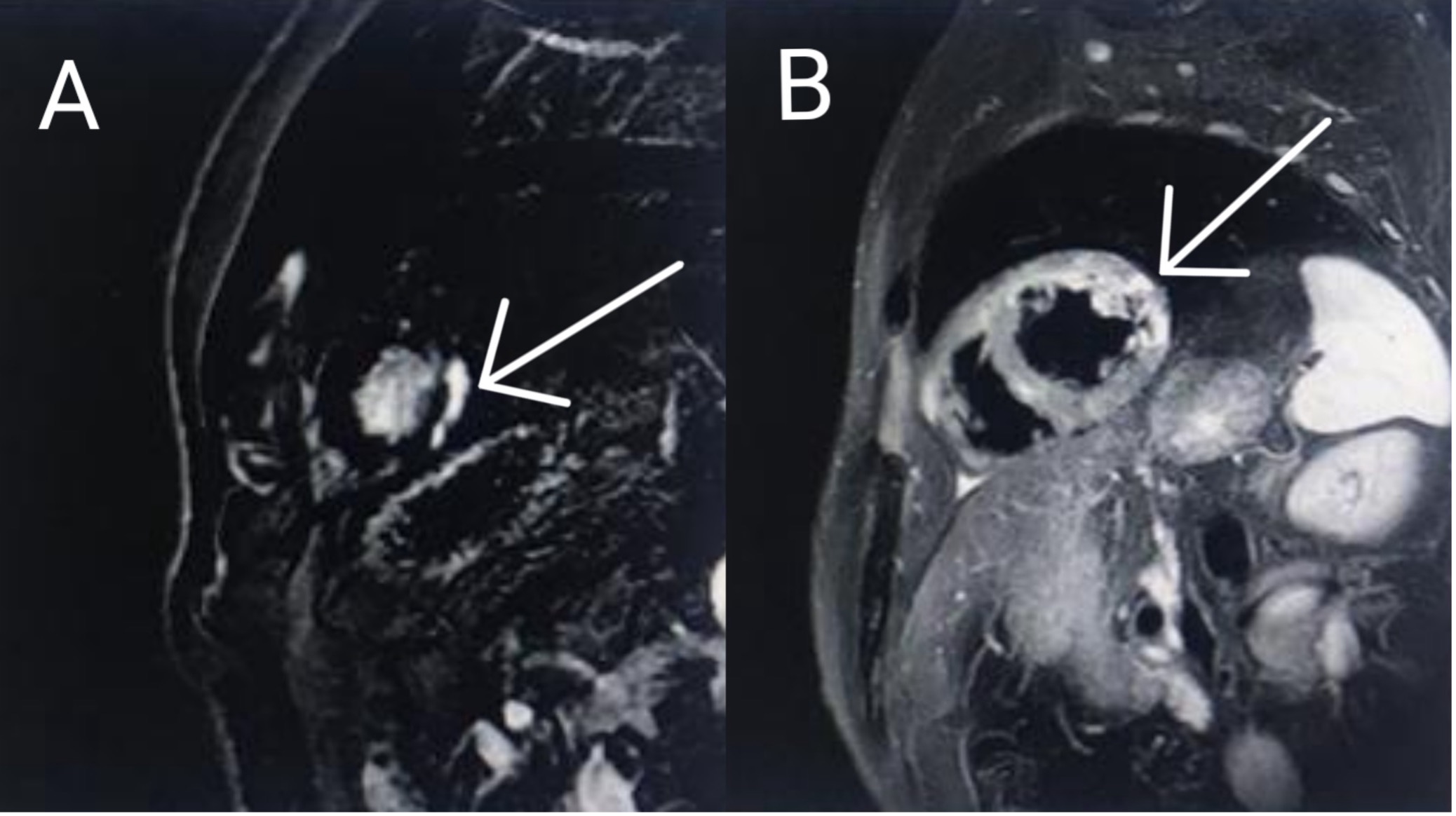
Case Report: A 54-year-old man admitted to the emergency department due to severe chest pain of two hours duration. Lab tests revealed high levels of troponin and D-dimer. ECG revealed tachycardia and ST-elevation in the anterolateral leads, making the diagnosis towards STEMI very likely. However, coronary angiogram didn’t show any obstruction in the right or left coronary arteries. Cardiac magnetic resonance (CMR) imaging was then performed and showed evidence of myocarditis. The patient was treated with colchicine and beta-blocker in which he showed a gradual recovery.
Conclusion: Our case highlights the difficulties that a physician may encounter when it comes to diagnosing a case of myocarditis. It should always be kept in mind when dealing with patients presenting with chest pain and ST-elevation, as it may mimic a typical STEMI presentation. A thorough clinical evaluation and the choice of appropriate diagnostic tools are key to the diagnosis of such challenging cases.
References
- Caforio AL, Pankuweit S, Arbustini E, et al. Current state of knowledge on aetiology, diagnosis, management, and therapy of myocarditis: a position statement of the European Society of Cardiology Working Group on Myocardial and Pericardial Diseases. Eur Heart J. 2013;34(33):2636-2648d. PMID: 23824828. Doi: https://doi.org/10.1093/eurheartj/eht210
- Fung G, Luo H, Qiu Y, Yang D, McManus B. Myocarditis. Circ Res. 2016;118(3):496-514. PMID: 26846643. Doi: https://doi.org/10.1161/CIRCRESAHA.115.306573
- Cooper LT Jr. Myocarditis. N Engl J Med. 2009;360(15):1526-1538. PMID: 19357408. PMCID: PMC5814110. Doi: https://doi.org/10.1056/NEJMra0800028
- Tschöpe C, Ammirati E, Bozkurt B, et al. Myocarditis and inflammatory cardiomyopathy: current evidence and future directions. Nat Rev Cardiol. 2021;18(3):169-193. PMID: 33046850. PMCID: PMC7548534 . Doi: https://doi.org/10.1038/s41569-020-00435-x
- Hufnagel G, Pankuweit S, Richter A, Schönian U, Maisch B. The European Study of Epidemiology and Treatment of Cardiac Inflammatory Diseases (ESETCID). First epidemiological results. Herz. 2000;25(3):279-285. PMID: 10904853. Doi: https://doi.org/10.1007/s000590050021
- Schultheiss HP, Kühl U, Cooper LT. The management of myocarditis. Eur Heart J. 2011;32(21):2616-2625. PMID: 21705357. Doi: https://doi.org/10.1093/eurheartj/ehr165
- Olejniczak M, Schwartz M, Webber E, Shaffer A, Perry TE. Viral Myocarditis-Incidence, Diagnosis and Management. J Cardiothorac Vasc Anesth. 2020;34(6):1591-1601. PMID: 32127272. Doi: https://doi.org/10.1053/j.jvca.2019.12.052
- Yilmaz A, Mahrholdt H, Athanasiadis A, et al. Coronary vasospasm as the underlying cause for chest pain in patients with PVB19 myocarditis. Heart. 2008;94(11):1456-1463. PMID: 18230640. Doi: https://doi.org/10.1136/hrt.2007.131383
- Sarda L, Colin P, Boccara F, et al. Myocarditis in patients with clinical presentation of myocardial in-farction and normal coronary angiograms. J Am Coll Cardiol. 2001;37(3):786-792. PMID: 11693753. Doi: https://doi.org/10.1016/s0735-1097(00)01201-8
- Friedrich MG, Sechtem U, Schulz-Menger J, et al. Cardiovascular magnetic resonance in myocarditis: A JACC White Paper. J Am Coll Cardiol. 2009;53(17):1475-1487. PMID: 19389557. PMCID: PMC2743893. Doi: https://doi.org/10.1016/j.jacc.2009.02.007
- Bozkurt B, Colvin M, Cook J, et al. Current Diagnostic and Treatment Strategies for Specific Dilated Cardiomyopathies: A Scientific Statement From the American Heart Association [published correction appears in Circulation. 2016 Dec 6;134(23 ):e652]. Circulation. 2016;134(23):e579-e646. PMID: 27832612. Doi: https://doi.org/10.1161/CIR.0000000000000455
Published
How to Cite
Issue
Section
Copyright (c) 2024 International Journal of Clinical Research

This work is licensed under a Creative Commons Attribution 4.0 International License.







