Vitamin D Deficiency Mimicking Pseudohypoparathyroidism Type II in an Adolescent Boy: A Case Report
DOI:
https://doi.org/10.38179/ijcr.v3i1.126Keywords:
hypocalcemia, pseudohypoparathyroidism, vitamin D deficiency, seizure, endocrinologyAbstract
Background: Vitamin D deficiency in children is common and usually characterized by hypocalcemia, hypophosphatemia, and elevated serum parathyroid hormone level. However, vitamin D deficiency can be associated with parathyroid hormone resistance in the kidneys which may cause hyperphosphatemia instead, mimicking thus pseudohypoparathyroidism type II. The exact pathogenesis for parathyroid hormone resistance remains unclear, and the distinction between the two conditions remains difficult. We describe the case of an adolescent who presented with seizures and was found to have biochemical features consistent with pseudohypoparathyroidism, likely related to vitamin D deficiency.
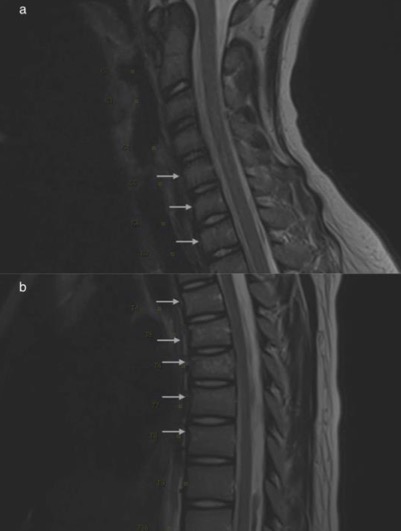
Case Report: A 13-year-old previously healthy adolescent presented with seizures. He experienced back pain during the previous month prior to the presentation. He did not have features of Albright hereditary osteodystrophy. His laboratory studies were significant for hypocalcemia, hyperphosphatemia, elevated serum alkaline phosphatase level, elevated parathyroid hormone level, and a deficient vitamin D level. Magnetic resonance imaging of the spine revealed multiple compression fractures. The child was treated with intravenous calcium and vitamin D administration with rapid improvement and his seizures resolved.
Conclusion: Hypocalcemia from vitamin D deficiency can mimic pseudohypoparathyroidism type II. The principles of treatment for hypocalcemia in both conditions are similar and patients require timely intervention with close follow-up to ensure the resolution of symptoms. Patients with resolution of symptoms after adequate treatment may not require further evaluation for other types of pseudohypoparathyroidism.
References
Murray TM, Rao LG, Divieti P, et al. Parathyroid Hormone Secretion and Action: Evidence for Discrete Receptors for the Carboxyl-Terminal Region and Related Biological Actions of Carboxyl-Terminal Ligands. Endocrine Reviews. 2005;26(1):78-113. PMID: 15689574. https://doi.org/10.1210/er.2003-0024.
Turan, S. Current Nomenclature of Pseudohypoparathyroidism: Inactivating Parathyroid Hormone/Parathyroid Hormone-Related Protein Signaling Disorder. Journal of Clinical Research in Pediatric Endocrinology. 2017;9(Suppl 2):58-68. PMID: 29280743. http://doi.org/10.4274/jcrpe.2017.S006.
Holick MF, Binkley NC, Bischoff-Ferrari HA, et al. Evaluation, treatment, and prevention of vitamin D deficiency: an Endocrine society clinical practice guideline. Journal of Clinical Endocrinology and Metabolism. 2011;96(7):1911-1930. PMID: 21646368. http://doi.org/10.1210/jc.2011-0385.
Underbjerg L, Sikjaer T, Mosekilde L, et al. Pseudohypoparathyroidism- epidemiology, mortality and risk of complications. Clinical Endocrinology. 2016;84(6):904-911. PMID: 26387561. http://doi.org/10.1111/cen.12948.
Mantovani G, Bastepe M, Monk D, et al. Diagnosis and management of pseudohypoparathyroidism and related disorders: first international Consensus Statement. Nature Reviews Endocrinology. 2018;14:476-500. PMID: 29959430. http://doi.org/10.1038/s41574-018-0042-0.
Cui W, Kobau R, Zack MM, et al. Seizures in Children and Adolescents Aged 6-17 Years- United States, 2010-2014. Morbidity and Mortality Weekly Report- CDC. 2015;64(43):1209-1214. PMID: 26540283. http://doi.org/10.15585/mmwr.mm6443a2.
Burgert T, Markowitz M. Understanding and Recognizing Pseudohypoparathyroidism. Pediatrics in Review. 2005(8);26:308-309. https://doi.org/10.1542/pir.26-8-308.
Felner EI, Marks JF, Germak JA. A variation of vitamin D deficiency in children. Journal of Pediatric Endocrinology and Metabolism. 2001;14(2):203-206. PMID: 11305799. http://doi.org/10.1515/jpem.2001.14.2.203.
Brook CG, Brown RS. Handbook of Clinical Pediatric Endocrinology First Edition. Malden, MA: Blackwell Publishing, Inc; 2008.
Misra M, Pacaud D, Petryk A, et al. Vitamin D Deficiency in Children and its Management: Review of Current Knowledge and Recommendations. Pediatrics. 2008;122(2):398-417. PMID: 18676559. http://doi.org/10.1542/peds.2007-1894.
Edouard T, Alos N, Chabot G, et al. Short- and long-term outcome of patients with pseudo-vitamin D deficiency rickets treated with calcitriol. Journal of Clinical Endocrinology and Metabolism. 2011;96(1):82-89. PMID: 20926527. http://doi.org/10.1210/jc.2010-1340.
Published
How to Cite
Issue
Section
Copyright (c) 2022 International Journal of Clinical Research

This work is licensed under a Creative Commons Attribution 4.0 International License.







