Iatrogenic Tracheal Injury During Endotracheal Tube Exchange in a COVID-19 Patient: A Case Report
DOI:
https://doi.org/10.38179/ijcr.v3i1.131Keywords:
Tracheoesophageal fistulas, tracheal injuries, tracheal inflammation, endotracheal tube exchange, COVID-19, neutrophil extracellular traps (NETs), Case ReportAbstract
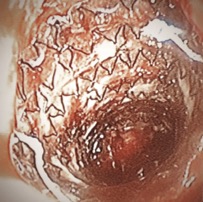
The coronavirus disease 2019 (COVID-19) pandemic has increased the need for prolonged intubation and mechanical ventilation. Though a rare complication of mechanical intubation, tracheoesophageal fistulas (TEFs) are severe and life-threatening. We present a patient with COVID-19 pneumonia who developed an iatrogenic TEF suspected to have been acquired during traumatic reintubation. After optimizing her for surgery, management of the TEF included tracheostomy tube placement at the distal end of the tracheal injury and placement of a stent over the defect. CT scan later showed migration of the stent into the esophagus that required removal. Despite receiving supportive therapy, the patients’ status declined and the patient shortly expired. By increasing demand for prolonged mechanical ventilation, complicating intubations amid fears of transmission, and potentially causing inflammatory tracheal damage, COVID-19 creates heightened obstacles to intubation that may put patients at risk of acquiring tracheal injuries. Increased awareness of possible tracheal injuries should be made by considering the many risk factors.
References
Bibas BJ, Cardoso PFG, Minamoto H, Pêgo-Fernandes PM. Surgery for intrathoracic tracheoesophageal and bronchoesophageal fistula. Ann Transl Med. 2018;6(11). PMID: 30023373. https://doi.org/10.21037/atm.2018.05.25
Kaloud H, Smolle-Juettner FM, Prause G, List WF. Iatrogenic ruptures of the tracheobronchial tree. Chest. 1997;112(3):774-778. PMID: 9315814. https://doi.org/10.1378/chest.112.3.774
Seegobin RD, van Hasselt GL. Endotracheal cuff pressure and tracheal mucosal blood flow: endoscopic study of effects of four large volume cuffs. Br Med J (Clin Res Ed). 1984;288(6422):965-968. PMID: 6423162. https://doi.org/10.1136/bmj.288.6422.965
Alkrekshi A, Bukamur H. Iatrogenic esophageal and tracheal perforation with tracheoesophageal fistula following emergency intubation. Clin Case Rep. 2020;9(1):588-589. PMID: 33489224. https://doi.org/10.1002/ccr3.3552
Mooty RC, Rath P, Self M, Dunn E, Mangram A. Review of tracheo-esophageal fistula associated with endotracheal intubation. J Surg Educ. 2007;64(4):237-240. PMID: 17706579. https://doi.org/10.1016/j.jsurg.2007.05.004
Bassi M, Anile M, Pecoraro Y, et al. Bedside Transcervical-Transtracheal Postintubation Injury Repair in a COVID-19 Patient. The Annals of Thoracic Surgery. 2020;110(5):e417-e419. PMID: 32333850. https://doi.org/10.1016/j.athoracsur.2020.04.009
Abou-Arab O, Huette P, Berna P, Mahjoub Y. Tracheal trauma after difficult airway management in morbidly obese patients with COVID-19. British Journal of Anaesthesia. 2020;125(1):e168-e170. PMID: 32334809. https://doi.org/10.1016/j.bja.2020.04.004
Kim HS, Khemasuwan D, Diaz-Mendoza J, Mehta AC. Management of tracheo-oesophageal fistula in adults. European Respiratory Review. 2020;29(158). PMID: 33153989. https://doi.org/10.1183/16000617.0094-2020
Ramai D, Bivona A, Latson W, et al. Endoscopic management of tracheoesophageal fistulas. Ann Gastroenterol. 2019;32(1):24-29. PMID: 30598588. https://doi.org/10.20524/aog.2018.0321
Rodríguez-Fuster A, Espases RA, Ventura JF, Bartolomé RA, Navas SS, Belda-Sanchis J. Tracheal trauma in the context of the current infection by COVID-19. About 2 cases. Arch Bronconeumol. 2020;56(10):670-671. PMID: 32586703. https://doi.org/10.1016/j.arbr.2020.08.007
Meister KD, Pandian V, Hillel AT, et al. Multidisciplinary Safety Recommendations After Tracheostomy During COVID-19 Pandemic: State of the Art Review. Otolaryngol Head Neck Surg. 2021;164(5):984-1000. PMID: 32960148. https://doi.org/10.1177/0194599820961990
Fiacchini G, Tricò D, Ribechini A, et al. Evaluation of the Incidence and Potential Mechanisms of Tracheal Complications in Patients With COVID-19. JAMA Otolaryngol Head Neck Surg. 2021;147(1):70-76. PMID: 33211087. https://doi.org/10.1001/jamaoto.2020.4148
Minonishi, T., Kinoshita, H., Hirayama, M., Kawahito, S., Azma, T., Hatakeyama, N., & Fujiwara, Y. The supine-to-prone position change induces modification of endotracheal tube cuff pressure accompanied by tube displacement. Journal of clinical anesthesia, 25(1), 28–31. PMID: 23391343. https://doi.org/10.1016/j.jclinane.2012.05.007
McGrath BA, Wallace S, Goswamy J. Laryngeal oedema associated with COVID-19 complicating airway management. Anaesthesia. 2020;75(7):972-972. PMID: 32302417. https://doi.org/10.1111/anae.15092
Rubano JA, Jasinski PT, Rutigliano DN, et al. Tracheobronchial Slough, a Potential Pathology in Endotracheal Tube Obstruction in Patients With Coronavirus Disease 2019 (COVID-19) in the Intensive Care Setting. Ann Surg. 2020;272(2):e63-e65. PMID: 32675499. https://doi.org/10.1097/SLA.0000000000004031
Polak SB, Van Gool IC, Cohen D, von der Thüsen JH, van Paassen J. A systematic review of pathological findings in COVID-19: a pathophysiological timeline and possible mechanisms of disease progression. Mod Pathol. Published online June 22, 2020:1-11. PMID: 32572155. https://doi.org/10.1038/s41379-020-0603-3
Oliver CM, Campbell M, Dulan O, Hamilton N, Birchall M. Appearance and management of COVID-19 laryngo-tracheitis: two case reports. F1000Res. 2020;9:310. PMID: 32724561. https://doi.org/10.12688/f1000research.23204.2
Veras FP, Pontelli MC, Silva CM, et al. SARS-CoV-2–triggered neutrophil extracellular traps mediate COVID-19 pathologySARS-CoV-2 directly triggers ACE-dependent NETs. Journal of Experimental Medicine. 2020;217(e20201129). PMID: 32926098. https://doi.org/10.1084/jem.20201129
Ward PA, Collier JM, Weir J, et al. Histological findings of tracheal samples from COVID-19 positive critically ill mechanically ventilated patients. Clinical Otolaryngology. n/a(n/a). PMID: 34606150. https://doi.org/10.1111/coa.13872
Published
How to Cite
Issue
Section
Copyright (c) 2022 International Journal of Clinical Research

This work is licensed under a Creative Commons Attribution 4.0 International License.







