Listeria Necrotizing Cellulitis: A Case Report
DOI:
https://doi.org/10.38179/ijcr.v3i1.135Keywords:
Listeria, Cellulitis, Necrotizing, Soft tissue infection, COVID-19Abstract
Background: L. monocytogenes typically affects pregnant women, neonates, or immunocompromised individuals, with a wide clinical spectrum that includes Central Nervous System (CNS) infections, endocarditis, and very rarely, localized infections such as necrotizing fasciitis . Although L. monocytogenes is the main pathogenic species, there are a total of 21 described species including L. grayi. L. grayi is not a well recognized human pathogen, despite a few case reports of infection in organ transplant patients. Listeria-associated soft tissue infections are exceedingly rare and are typically seen in immunocompromised individuals, with the usual culprit being Listeria monocytogenes.
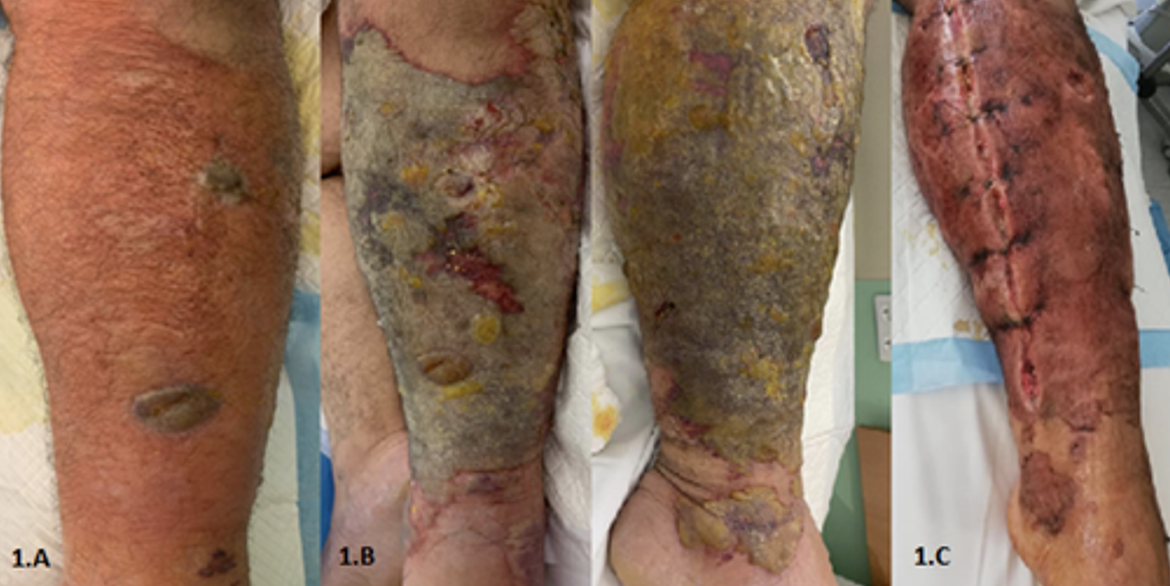
Case Report: We report the case of A 33-year-old previously healthy male, presented to the Emergency Department (ED) with left leg swelling, erythema, and fever. After multiple courses of treatment, we were able to isolate the L.grayi from the intraoperative specimen, confirmed the diagnosis of L.grayi associated cellulitis in a healthy young non-immunocompromised patient.
Conclusion: This is to the best of our knowledge the first case of Listeria Grayi associated soft tissue infection in a previously healthy young man 3 months after recovery from COVID-19 infection.
References
Nwaiwu O. What are the recognized species of the genus Listeria?. Access Microbiol. 2020;2(9):acmi000153. Published 2020 Jul 21. PMID: 33195982. https://doi.org/10.1099%2Facmi.0.000153
Libanore M, Merlo R, Borin M, et al. Listeria Monocytogenes: an uncommon pathogen of cervical necrotizing fasciitis. B-ENT. 2016;12(3):245-247. PMID: 29727131.
Sendi P, Marti E, Fröhlicher S, Constantinescu MA, Zimmerli S. Necrotizing Fasciitis due to Listeria monocytogenes. Clin Infect Dis. 2009;48(1):138-139. https://doi.org/10.1086/595974
Rapose A, Lick SD, Ismail N. Listeria grayi bacteremia in a heart transplant recipient. Transpl Infect Dis. 2008;10(6):434-436. PMID: 18811634. https://doi.org/10.1111/j.1399-3062.2008.00333.x
Salimnia H, Patel D, Lephart PR, Fairfax MR, Chandrasekar PH. Listeria grayi: vancomycin-resistant, gram-positive rod causing bacteremia in a stem cell transplant recipient. Transpl Infect Dis. 2010;12(6):526-528. PMID: 20626713. https://doi.org/10.1111/j.1399-3062.2010.00539.x
Wellinghausen N. Listeria and Erysipelothrix. In: Jorgensen JH, Carroll KC, Funke G, et al., eds. Manual of Clinical Microbiology. ASM Press; 2015:462-473. https://doi.org/10.1128/9781555817381.ch27
Vital Signs: Listeria Illnesses, Deaths, and Outbreaks — United States, 2009–2011. CDC. 2021. https://www.cdc.gov/mmwr/preview/mmwrhtml/mm6222a4.htm
Swaminathan B, Gerner-Smidt P. The epidemiology of human listeriosis. Microbes Infect. 2007;9(10):1236-1243. PMID: 17720602. https://doi.org/10.1016/j.micinf.2007.05.011
Godshall CE, Suh G, Lorber B. Cutaneous listeriosis. J Clin Microbiol. 2013;51(11):3591-3596. PMID: 23966491. https://doi.org/10.1128%2FJCM.01974-13
Todeschini G, Friso S, Lombardi S, Casaril M, Fontana R, Corrocher R. A case of Listeria murray/grayi bacteremia in a patient with advanced Hodgkin's disease. Eur J Clin Microbiol Infect Dis. 1998;17(11):808-810. PMID: 9923527. https://doi.org/10.1007/s100960050193
Otto M. Staphylococcus epidermidis--the 'accidental' pathogen. Nat Rev Microbiol. 2009;7(8):555-567. PMID: 19609257. https://doi.org/10.1038%2Fnrmicro2182
Published
How to Cite
Issue
Section
Copyright (c) 2022 International Journal of Clinical Research

This work is licensed under a Creative Commons Attribution 4.0 International License.







