Clinical Correlation Between Pre and Post ERCP Laboratory Values
DOI:
https://doi.org/10.38179/ijcr.v3i1.166Keywords:
Endoscopy, Endoscopic retrograde cholangiopancreatography, Pancreatitis, Cholangitis, Choledocholithiasis, Biliary sphincterotomy, StrictureAbstract
Background: Endoscopic retrograde cholangiopancreatography (ERCP) has evolved from a diagnostic modality to a primarily therapeutic procedure for pancreatic as well as biliary disorders. However, several complications were described post-procedure such as pancreatitis, perforation, cholangitis, post-sphincterotomy bleeding, etc. Data concerning variation in laboratory values before and after ERCP and its clinical significance with respect to endoscopic findings and possible complications is lacking in the literature.
Aim: To analyze the clinical significance of laboratory values in patients before and after ERCP.
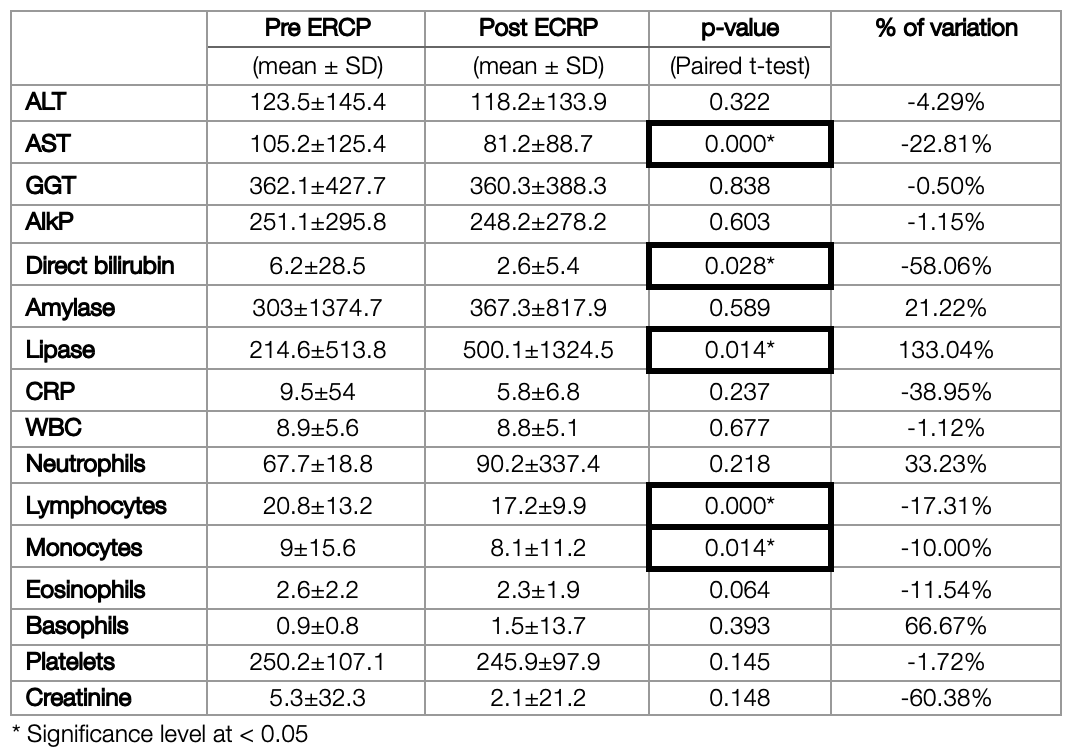
Methods: From a total of 723 patients, 363 with different sets of findings on ERCP were eligible to be included in the study and were divided into 8 different groups. Serum levels of alanine aminotransferase (ALT), aspartate aminotransferase (AST), Gamma-glutamyl transferase (GGT), Alkaline phosphatase (ALKP), bilirubin, amylase, lipase, c-reactive protein (CRP), white blood count (WBC), neutrophil, lymphocyte, monocyte, eosinophils, basophils, platelets counts and creatinine were determined preoperatively as well as postoperatively in these patients.
Results: AST and direct bilirubin showed a significant difference in all patients between pre and post-ERCP (p-value<0.01 and p-value<0.05, respectively). Liver tests were significantly higher in the malignant obstruction group than in the bile duct stones group (P <0.05) and decrease more significantly (P <0.05) after the procedure. A significant increase in lipase (p-value<0.05) among all groups was found, and interestingly, the lymphocytic count showed a significant decrease (p-value<0.01).
Conclusion: In conclusion, (1) ERCP significantly decreases AST, direct bilirubin, lymphocytes, and monocytes count post procedure among all stratified groups of obstructive etiology thus proving its therapeutic value for biliary system obstructions. (2) Higher baseline disturbances in laboratory values at T0, especially in liver function tests such as ALT, AST, GGT, and ALKP as well as a bigger decrease in lymphocyte count at T1 are noted to be linked with malignant obstructions (tumor group), rather than benign obstructions (stone, sludge, stone+ sludge, and stricture). (3) Finally, stone and stricture groups are at the highest risk of post-ERCP pancreatitis owing to those groups having the highest pancreatic enzyme levels post ERCP, and thus should be the best candidates for a pre-ERCP pharmacologic prophylaxis (such as diclofenac, etc) and post ERCP close monitoring.
References
Khamaysi I, Taha R. ERCP for severe acute cholangitis: The earlier, the better. Turk J Gastroenterol. 2020;31(1):78-79. PMID: 32009619. https://doi.org/10.5152%2Ftjg.2020.19103
Khamaysi I, Taha R. ERCP for severe acute cholangitis: The earlier, the better. Turk J Gastroenterol. 2020;31(1):78-79. PMID: 32009619. https://doi.org/10.5152%2Ftjg.2020.19103
Meseeha M, Attia M. Endoscopic Retrograde Cholangiopancreatography. In: StatPearls. Treasure Island (FL): StatPearls Publishing; May 10, 2022. PMID: 29630212.
Talukdar R. Complications of ERCP. Best Pract Res Clin Gastroenterol. 2016;30(5):793-805. PMID: 27931637. https://doi.org/10.1016/j.bpg.2016.10.007
Tan M, Schaffalitzky de Muckadell OB, Laursen SB. Association between early ERCP and mortality in patients with acute cholangitis. Gastrointest Endosc. 2018;87(1):185-192. PMID: 28433613. https://doi.org/10.1016/j.gie.2017.04.009
Al Quorain A, Ibrahim EM, Al Sultan AI. Diagnostic and therapeutic value of ERCP and prediction of outcome: a retrospective analysis. Saudi J Gastroenterol. 1996;2(3):138-141. PMID: 19864821.
Ott DJ, Young GP, Mitchell RG, Chen MY, Gelfand DW. Therapeutic ERCP: spectrum of procedures performed in 60 consecutive patients. Abdom Imaging. 1994;19(1):30-33. PMID: 8161899. https://doi.org/10.1007/bf02165857
Song, W. & Bo, P. & Chen, C.-W & Liu, J. & Deng, D.-H & Chen, J. Clinical significance of liver function indexes in patients before and after ERCP. Wrld Chinese Jrnl of Dgtl. 2013. http://dx.doi.org/10.11569/wcjd.v21.i18.1772
Yu CY, Roth N, Jani N, et al. Dynamic liver test patterns do not predict bile duct stones. Surg Endosc. 2019;33(10):3300-3313. PMID: 30911921. https://doi.org/10.1007/s00464-018-06620-x
Andriulli A, Loperfido S, Napolitano G, et al. Incidence rates of post-ERCP complications: a systematic survey of prospective studies. Am J Gastroenterol. 2007;102(8):1781-1788. PMID: 17509029. https://doi.org/10.1111/j.1572-0241.2007.01279.x
Panda C, Das H, et al. Chitta Ranjan et al. Retrospective analysis of endoscopic retrograde cholangio pancreatography (ERCP) procedures in a tertiary care centre in coastal Odisha. International Journal of Research in Medical Sciences. 2017. http://dx.doi.org/10.18203/2320-6012.ijrms20174113.
Cotton PB, Garrow DA, Gallagher J, Romagnuolo J. Risk factors for complications after ERCP: a multivariate analysis of 11,497 procedures over 12 years. Gastrointest Endosc. 2009;70(1):80-88. PMID: 19286178. https://doi.org/10.1016/j.gie.2008.10.039
Barthet M, Lesavre N, Desjeux A, et al. Complications of endoscopic sphincterotomy: results from a single tertiary referral center. Endoscopy. 2002;34(12):991-997. PMID: 12471544. https://doi.org/10.1055/s-2002-35834
Vandervoort J, Soetikno RM, Tham TC, et al. Risk factors for complications after performance of ERCP. Gastrointest Endosc. 2002;56(5):652-656. PMID: 12397271. https://doi.org/10.1067/mge.2002.129086
Lv ZH, Kou DQ, Guo SB. Three-hour post-ERCP amylase level: a useful indicator for early prediction of post-ERCP pancreatitis. BMC Gastroenterol. 2020;20(1):118. Published 2020 Apr 20. PMID: 32306904. https://doi.org/10.1186%2Fs12876-020-01254-7
Geraci G, Palumbo VD, D'Orazio B, Maffongelli A, Fazzotta S, Lo Monte AI. Rectal Diclofenac administration for prevention of post-Endoscopic Retrograde Cholangio-Pancreatography (ERCP) acute pancreatitis. Randomized prospective study. Clin Ter. 2019;170(5):e332-e336. PMID: 31612188. https://doi.org/10.7417/ct.2019.2156
Published
How to Cite
Issue
Section
Copyright (c) 2022 International Journal of Clinical Research

This work is licensed under a Creative Commons Attribution 4.0 International License.