Pleural Effusion Associated with Ulcerative Colitis: A Case Report
DOI:
https://doi.org/10.38179/ijcr.v3i1.197Keywords:
Ulcerative Colitis, Pleural Effusion, Mesalamine, Case ReportAbstract
Background: Extraintestinal manifestations associated with IBD may involve the skin, joints, hepatobiliary tract, eye, kidney, and rarely pancreas and respiratory systems; as well as risks for venous thrombosis. They may be present at diagnosis or develop later in the disease course. Pulmonary complications of IBD include airway inflammation, parenchymal lung disease, serositis, thromboembolic disease, and drug-induced lung toxicity.
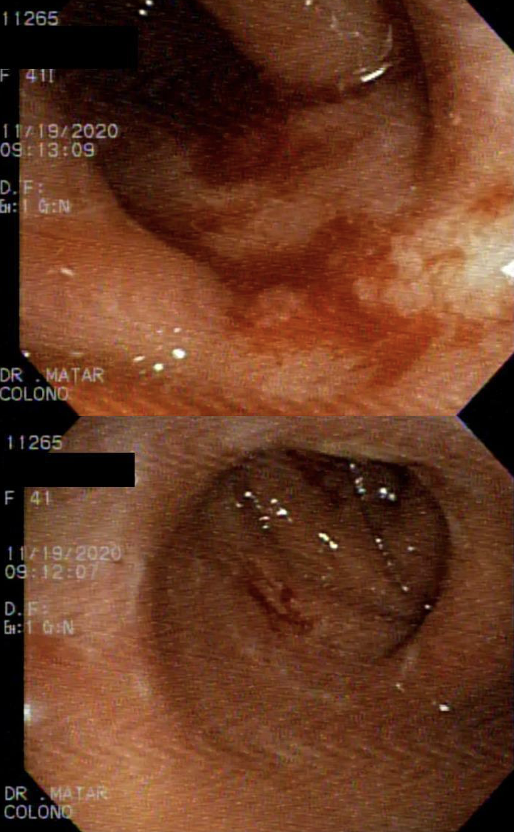
Case Presentation: We report a case of a 41-year-old lady with ulcerative colitis who presented to the hospital with respiratory symptoms. Physical examination and imagery lead to the diagnosis of acute pleural effusion. Later on, the patient developed gastrointestinal symptoms. Colonoscopy and biopsy showed that she has Ulcerative Colitis. Which is a very rare presentation of EIM of IBD. The patient improved on steroids and mesalamine and pleural effusion resolved.
Conclusion: In conclusion, pulmonary involvement should be considered when pleurisy develops in UC. Early diagnosis and effective treatment are important for these patients.
References
The Facts About Inflammatory Bowel Diseases. New York, NY: Crohn’s and Colitis Foundation of America; 2014. http://www.crohnscolitisfoundation.org/assets/pdfs/updatedibdfactbook.pdf
Rankin GB. Extraintestinal and systemic manifestations of inflammatory bowel disease. Med Clin North Am. 1990;74(1):39-50. https://doi.org/10.1016/s0025-7125(16)30585-5. PMID: 2404180
Levine JS, Burakoff R. Extraintestinal manifestations of inflammatory bowel disease. Gastroenterol Hepatol (N Y). 2011;7(4):235-241. PMID: 21857821
Camus P, Piard F, Ashcroft T, Gal AA, Colby TV. The lung in inflammatory bowel disease. Medicine (Baltimore). 1993;72(3):151-183. PMID: 8502168
Black H, Mendoza M, Murin S. Thoracic manifestations of inflammatory bowel disease. Chest. 2007;131(2):524-532. https://doi.org/10.1378/chest.06-1074. PMID: 17296657
van Lierop PP, Samsom JN, Escher JC, Nieuwenhuis EE. Role of the innate immune system in the pathogenesis of inflammatory bowel disease. J Pediatr Gastroenterol Nutr. 2009;48(2):142-151. https://doi.org/10.1097/mpg.0b013e3181821964. PMID: 19179875
Higenbottam T, Cochrane GM, Clark TJ, Turner D, Millis R, Seymour W. Bronchial disease in ulcerative colitis. Thorax. 1980;35(8):581-585. https://doi.org/10.1136/thx.35.8.581. PMID: 7444824
Bonniere P, Wallaert B, Cortot A, et al. Latent pulmonary involvement in Crohn's disease: biological, functional, bronchoalveolar lavage and scintigraphic studies. Gut. 1986;27(8):919-925. https://doi.org/10.1136/gut.27.8.919. PMID: 3015749
Wallaert, B., Colombel, J. F., Tonnel, A. B., Bonniere, P. H., Cortot, A., Paris, J. C., & Voisin, C. (1985). Evidence of lymphocyte alveolitis in Crohn's disease. Chest, 87(3), 363-367. https://doi.org/10.1378/chest.87.3.363
Ji XQ, Wang LX, Lu DG. Pulmonary manifestations of inflammatory bowel disease. World J Gastroenterol. 2014 Oct 7;20(37):13501-11. https://doi.org/10.3748%2Fwjg.v20.i37.13501. PMID: 25309080
Barrecheguren M, Pons J, Trujillo G, et al. Bronchiectasis in ulcerative colitis: a case report. Respir Med Case Rep. 2020 Oct 3;31:101296. https://doi:10.1016/j.rmcr.2020.101296. PMID: 33083374
Li L, Liu P, Niu X, He C. Interstitial Lung Disease as an Extraintestinal Manifestation of Crohn’s Disease in the Time of COVID-19: A Rare Case Report and Review of the Literature. Journal of inflammation research. https://doi.org/10.2147/jir.s380879. PMID: 36238767
Taveras NT, Martinez AR, Kumar R, Jamil A, Kumar B. Pulmonary manifestations of inflammatory bowel disease. Cureus. 2021 Mar 31;13(3). https://doi.org/10.7759%2Fcureus.14216. PMID: 33948406
Kraft SC, Earle RH, Roesler M, Esterly JR. Unexplained Bronchopulmonary Disease With Inflammatory Bowel Disease. Arch Intern Med. 1976;136(4):454–459. PMID: 1267553
Betancourt SL, Palacio D, Jimenez CA, Martinez S, Marom EM. Thoracic manifestations of inflammatory bowel disease. AJR Am J Roentgenol. 2011;197(3):W452-W456. https://doi.org/10.2214/ajr.10.5353. PMID: 21862772
Douglas, J. G., McDonald, C. F., Leslie, M. J., Gillon, J., Crompton, G. K., & McHardy, G. J. R. (1989). Respiratory impairment in inflammatory bowel disease: does it vary with disease activity? Respiratory medicine, 83(5), 389-394. https://doi.org/10.1016/s0954-6111(89)80070-8. PMID: 2616823
Loftus EV Jr. Clinical epidemiology of inflammatory bowel disease: Incidence, prevalence, and environmental influences. Gastroenterology. 2004;126(6):1504-1517. PMID: 15168363. https://doi.org/10.1053/j.gastro.2004.01.063
Hoffmann RM, Kruis W. Rare extraintestinal manifestations of inflammatory bowel disease. Inflamm Bowel Dis. 2004;10(2):140-147. https://doi.org/10.1097/00054725-200403000-00013. PMID: 15168815
Mahadeva R, Walsh G, Flower CD, Shneerson JM. Clinical and radiological characteristics of lung disease in inflammatory bowel disease. Eur Respir J. 2000;15(1):41-48. https://doi.org/10.1183/09031936.00.15104100. PMID: 10678619
Williams, H., Walker, D., & Orchard, T. R. (2008). Extraintestinal manifestations of inflammatory bowel disease. Current gastroenterology reports, 10(6), 597-605. https://doi.org/10.1007/s11894-008-0108-6
Kuzniar, T., Sleiman, C., Brugière, O., Groussard, O., Mal, H., Mellot, F., ... & Fournier, M. (2000). Severe tracheobronchial stenosis in a patient with Crohn's disease. European Respiratory Journal, 15(1), 209-212. https://doi.org/1034/j.1399-3003.2000.15a38.x
Porcel JM. Biomarkers in the diagnosis of pleural diseases: a 2018 update. Ther Adv Respir Dis. 2018;12:1753466618808660. https://doi.org/10.1177/1753466618808660. PMID: 30354850
Published
How to Cite
Issue
Section
Copyright (c) 2022 International Journal of Clinical Research

This work is licensed under a Creative Commons Attribution 4.0 International License.







