Risk Factors for Invasive Fungal Disease in Pediatric Oncology
DOI:
https://doi.org/10.38179/ijcr.v3i1.202Keywords:
invasive fungal disease, risk factors, pediatric oncology, mucositis, severe lymphopenia, chemotherapy intensity, acute myeloid leukemiaAbstract
Background: Invasive fungal infections are a major cause of death in pediatric oncology, especially among patients under chemotherapy. This study aims to identify risk factors for invasive fungal infections in pediatric oncology.
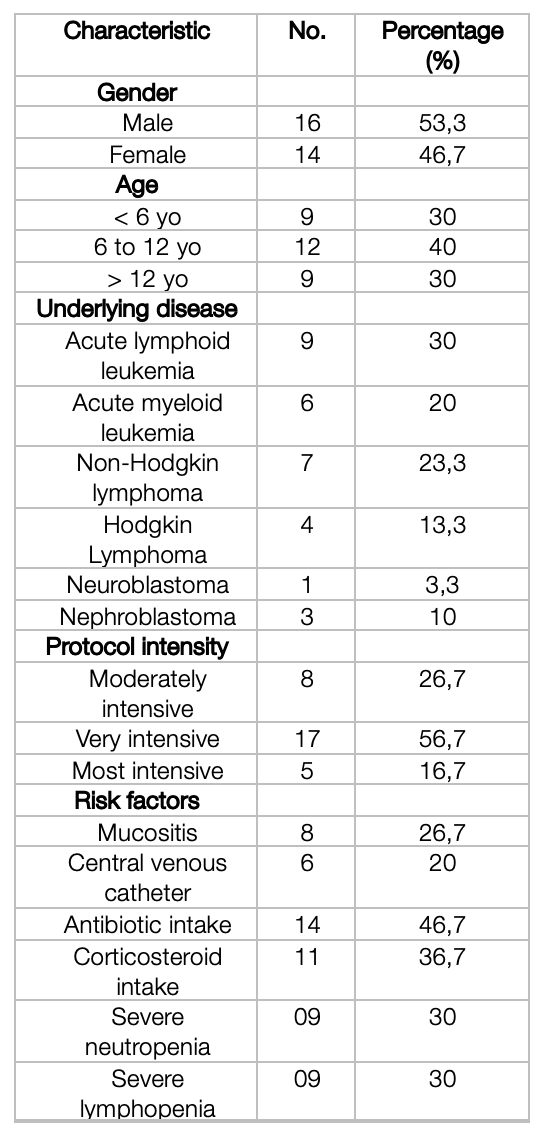
Methods: We conducted a monocentric retrospective case-control multi-cohort study on a population of 30 patients with malignant hemopathies or solid cancers under chemotherapy, admitted in the Pediatric Oncology unit of Nafissa Hammoud Hospital in Algiers, amongst which 24 patients were controls, and 6 patients were cases.
Results: In a total of 30 patients (53.3 % male), 13 patients developed a fever, from which 6 patients were identified as invasive fungal infection cases according to the European Organization for Research and Treatment of Cancer/Invasive Fungal Infections Cooperative Group and Infectious Diseases Mycoses Study Group (EORTC/MSG) guidelines, with an incidence of 20 %. The mean age was 7.47 years old at the admission date. Four statistically significant risk factors were identified (p-value < 0.05, CI 95 %): mucositis with an odds ratio (OR) at 10 (1,34 – 74,51), the most aggressive chemotherapy protocol according to the ITR2 with an OR at 115 (6,10 – 2165,95), severe prolonged neutropenia with an OR at 7,6 (1,07 – 54,09) and severe prolonged lymphopenia with an OR at 25 (2,27 – 275,71).
Conclusion: Many conditions were identified as risk factors for invasive fungal infections in pediatric oncology, especially severe lymphopenia and aggressive chemotherapy. These patients may have to receive close monitoring or even antifungal prophylaxis.
References
Pana ZD, Roilides E, Warris A, Groll AH, Zaoutis T. Epidemiology of Invasive Fungal Disease in Children. Journal of the Pediatric Infectious Diseases Society. 2017;6(suppl_1):S3-S11. PMID: 28927200. https://doi.org/10.1093/jpids/pix046
Lehrnbecher T, Schöning S, Poyer F, et al. Incidence and Outcome of Invasive Fungal Diseases in Children With Hematological Malignancies and/or Allogeneic Hematopoietic Stem Cell Transplantation: Results of a Prospective Multicenter Study. Front Microbiol. 2019;10:681. Published 2019 Apr 16. PMID: 31040830. https://doi.org/10.3389/fmicb.2019.00681
Rosen GP, Nielsen K, Glenn S, Abelson J, Deville J, Moore TB. Invasive fungal infections in pediatric oncology patients: 11-year experience at a single institution. J Pediatr Hematol Oncol. 2005;27(3):135-140. PMID: 15750444. https://doi.org/10.1097/01.mph.0000155861.38641.ca
Cesaro S, Tridello G, Castagnola E, et al. Retrospective study on the incidence and outcome of proven and probable invasive fungal infections in high-risk pediatric onco-hematological patients. Eur J Haematol. 2017;99(3):240-248. PMID: 28556426. https://doi.org/10.1111/ejh.12910
Muggeo P, Calore E, Decembrino N, et al. Invasive mucormycosis in children with cancer: A retrospective study from the Infection Working Group of Italian Pediatric Hematology Oncology Association. Mycoses. 2019;62(2):165-170. PMID: 30338581. https://doi.org/10.1111/myc.12862
Kazakou N, Vyzantiadis TA, Gambeta A, et al. Invasive fungal infections in a pediatric hematology-oncology department: A 16-year retrospective study. Curr Med Mycol. 2020;6(2):37-42. PMID: 33628980. https://dx.doi.org/10.18502%2FCMM.6.2.2840
Fisher BT, Robinson PD, Lehrnbecher T, et al. Risk Factors for Invasive Fungal Disease in Pediatric Cancer and Hematopoietic Stem Cell Transplantation: A Systematic Review. J Pediatric Infect Dis Soc. 2018;7(3):191-198. PMID: 28549148. https://doi.org/10.1093/jpids/pix030
Ascioglu S, Rex JH, de Pauw B, et al. Defining opportunistic invasive fungal infections in immunocompromised patients with cancer and hematopoietic stem cell transplants: an international consensus. Clin Infect Dis. 2002;34(1):7-14. PMID: 11731939. https://doi.org/10.1086/323335
De Pauw B, Walsh TJ, Donnelly JP, et al. Revised definitions of invasive fungal disease from the European Organization for Research and Treatment of Cancer/Invasive Fungal Infections Cooperative Group and the National Institute of Allergy and Infectious Diseases Mycoses Study Group (EORTC/MSG) Consensus Group. Clin Infect Dis. 2008;46(12):1813-1821. PMID: 18462102. https://doi.org/10.1086/588660
Donnelly JP, Chen SC, Kauffman CA, et al. Revision and Update of the Consensus Definitions of Invasive Fungal Disease From the European Organization for Research and Treatment of Cancer and the Mycoses Study Group Education and Research Consortium. Clin Infect Dis. 2020;71(6):1367-1376. PMID: 31802125. https://doi.org/10.1093/cid/ciz1008
Werba BE, Hobbie W, Kazak AE, Ittenbach RF, Reilly AF, Meadows AT. Classifying the intensity of pediatric cancer treatment protocols: the intensity of treatment rating scale 2.0 (ITR-2). Pediatr Blood Cancer. 2007;48(7):673-677. PMID: 17427232. https://doi.org/10.1002/pbc.21184
Villarroel M, Avilés CL, Silva P, et al. Risk factors associated with invasive fungal disease in children with cancer and febrile neutropenia: a prospective multicenter evaluation. Pediatr Infect Dis J. 2010;29(9):816-821. PMID: 20616763. https://doi.org/10.1097/inf.0b013e3181e7db7f
Mor M, Gilad G, Kornreich L, Fisher S, Yaniv I, Levy I. Invasive fungal infections in pediatric oncology. Pediatr Blood Cancer. 2011;56(7):1092-1097. PMID: 21319281. https://doi.org/10.1002/pbc.23005
Castagnola E, Cesaro S, Giacchino M, et al. Fungal infections in children with cancer: a prospective, multicenter surveillance study. Pediatr Infect Dis J. 2006;25(7):634-639. PMID: 16804435. https://doi.org/10.1097/01.inf.0000220256.69385.2e
Kobayashi R, Hori D, Sano H, Suzuki D, Kishimoto K, Kobayashi K. Risk Factors for Invasive Fungal Infection in Children and Adolescents With Hematologic and Malignant Diseases: A 10-year Analysis in a Single Institute in Japan. Pediatr Infect Dis J. 2018;37(12):1282-1285. PMID: 30408007. https://doi.org/10.1097/inf.0000000000002010
Ozsevik SN, Sensoy G, Karli A, et al. Invasive fungal infections in children with hematologic and malignant diseases. J Pediatr Hematol Oncol. 2015;37(2):e69-e72. PMID: 25072372. https://doi.org/10.1097/mph.0000000000000225
Lalla RV, Latortue MC, Hong CH, et al. A systematic review of oral fungal infections in patients receiving cancer therapy. Support Care Cancer. 2010;18(8):985-992. PMID: 20449755. https://doi.org/10.1007/s00520-010-0892-z
Bishop JF, Matthews JP, Young GA, et al. A randomized study of high-dose cytarabine in induction in acute myeloid leukemia. Blood. 1996;87(5):1710-1717. PMID: 8634416. https://doi.org/10.1182/blood.V87.5.1710.1710
Lanternier F, Cypowyj S, Picard C, et al. Primary immunodeficiencies underlying fungal infections. Curr Opin Pediatr. 2013;25(6):736-747. PMID: 24240293. https://dx.doi.org/10.1097%2FMOP.0000000000000031
Published
How to Cite
Issue
Section
Copyright (c) 2022 International Journal of Clinical Research

This work is licensed under a Creative Commons Attribution 4.0 International License.







