Permanent Pacemaker Use in Transcatheter Aortic Valve Replacement: Real World Experience from the National Inpatient Sample
DOI:
https://doi.org/10.38179/ijcr.v3i1.219Keywords:
TAVR, Permanent Pacemaker, National Inpatient SampleAbstract
Background: Transcatheter Aortic Valve Replacement (TAVR) is associated with conduction abnormalities requiring permanent pacemaker implantation (PPMI). Data regarding predictors for PPMI following TAVR is scarce.
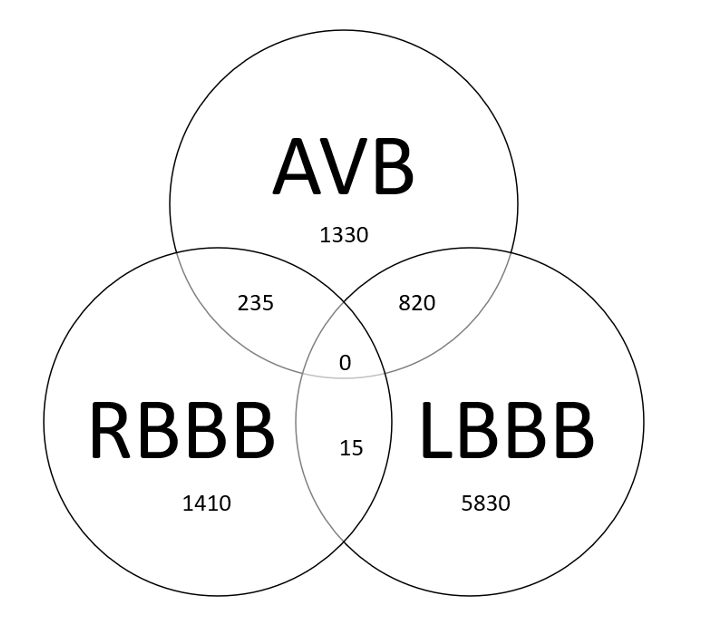
Methods: This is a retrospective study utilizing the 2017 National In-Patient Sample (NIS). Patients who underwent TAVR and PPMI during the same admission were identified using appropriate ICD-10 codes, as were patients with left bundle branch (LBBB), right bundle branch (RBBB), and first-degree AV delay (AVB). Patients were split into two groups based on PPMI. The groups were compared using univariate and multivariate analyses after adjusting for age, gender, race, comorbidities, insurance status, and Charlson comorbidity index (CCI). Secondary outcomes included factors influencing length of stay (LOS) and total charges incurred.
Results: In 2017, 54,175 (57.6% males) patients underwent TAVR. There were 8,067 patients with LBBB, 2,402 with RBBB, and 2,905 with AVB at baseline. A 4170 total of patients (55.2% males) required PPMI. Patients requiring PPMI were older (80.5 vs 79.6 years, p=0.001). On multivariate analyses, baseline RBBB, LBBB, hypertension (HTN), CCI 2, and CCI >/=3 predicted PPMI (aOR 4.82, p<0.001; aOR 1.63, p<0.001; aOR 1.21, p=0.013, aOR 1.53, p=0.022 and aOR 1.46, p=0.031 respectively). On multivariate analyses, patients who underwent PPMI had significantly higher LOS (aOR 2.18, p<0.001) and incurred higher total charges (USD 278,000 vs USD 204,920; p<0.001).
Conclusion: In this cohort, RBBB, LBBB, HTN, and increased CCI predicted PPMI after TAVR. Further studies are required to corroborate our findings.
References
Leon MB, Smith CR, Mack M, et al. Transcatheter aortic-valve implantation for aortic stenosis in patients who cannot undergo surgery. N Engl J Med. 2010;363(17):1597-1607. PMID: 20961243 https://www.nejm.org/doi/full/10.1056/nejmoa1008232
Popma JJ, Deeb GM, Yakubov SJ, et al. Transcatheter Aortic-Valve Replacement with a Self-Expanding Valve in Low-Risk Patients. N Engl J Med. 2019;380(18):1706-1715. PMID: 30883503 https://www.nejm.org/doi/full/10.1056/nejmoa1816885
Mack MJ, Leon MB, Thourani VH, et al. Transcatheter Aortic-Valve Replacement with a Balloon-Expandable Valve in Low-Risk Patients. N Engl J Med. 2019;380(18):1695-1705. PMID: 30883508 https://www.nejm.org/doi/full/10.1056/nejmoa1814052
Leon MB, Smith CR, Mack MJ, et al. Transcatheter or Surgical Aortic-Valve Replacement in Intermediate-Risk Patients. N Engl J Med. 2016;374(17):1609-1620. PMID: 27040324 https://www.nejm.org/doi/full/10.1056/nejmoa1514616
Smith CR, Leon MB, Mack MJ, et al. Transcatheter versus Surgical Aortic-Valve Replacement in High-Risk Patients. N Engl J Med. 2011;364(23):2187-2198. PMID: 21639811 https://www.nejm.org/doi/full/10.1056/nejmoa1103510
Sammour Y, Krishnaswamy A, Kumar A, et al. Incidence, Predictors, and Implications of Permanent Pacemaker Requirement After Transcatheter Aortic Valve Replacement. JACC Cardiovasc Interv. 2021;14(2):115-134. PMID:33478630 https://www.jacc.org/doi/abs/10.1016/j.jcin.2020.09.063
Siontis GCM, Jüni P, Pilgrim T, et al. Predictors of Permanent Pacemaker Implantation in Patients With Severe Aortic Stenosis Undergoing TAVR. Am Coll Cardiol. 2014;64(2):129-140. PMID: 25011716 https://www.jacc.org/doi/abs/10.1016/j.jacc.2014.04.033
Nazif TM, Dizon José M, Hahn RT, et al. Predictors and Clinical Outcomes of Permanent Pacemaker Implantation After Transcatheter Aortic Valve Replacement. JACC Cardiovasc In-terv. 2015;8(1):60-69. PMID: 25616819 https://www.jacc.org/doi/abs/10.1016/j.jcin.2014.07.022
Bisson A, Bodin A, Herbert J, et al. Pacemaker Implantation After Balloon‐ or Self‐Expandable Transcatheter Aortic Valve Replacement in Patients With Aortic Stenosis. J Am Heart Assoc. 2020;9(9). PMID: 32362220 https://www.ahajournals.org/doi/10.1161/JAHA.120.015896
Mazzella AJ, Hendrickson MJ, Arora S, et al. Shifting Trends in Timing of Pacemaker Implantation After Transcatheter Aortic Valve Replacement. JACC Cardiovasc Interv. 2021;14(2):232-234.PMID: 33183993 https://www.jacc.org/doi/abs/10.1016/j.jcin.2020.09.034
ROTEN L, STORTECKY S, SCARCIA F, et al. Atrioventricular Conduction After Transcatheter Aortic Valve Implantation and Surgical Aortic Valve Replacement. J Car-diovasc Electrophysiol. 2012;23(10):1115-1122. PMID: 22587564 https://onlinelibrary.wiley.com/doi/10.1111/j.1540-8167.2012.02354.x
Bagur R, Rodés-Cabau J, Gurvitch R, et al. Need for Permanent Pacemaker as a Com-plication of Transcatheter Aortic Valve Implantation and Surgical Aortic Valve Replace-ment in Elderly Patients With Severe Aortic Stenosis and Similar Baseline Electrocardi-ographic Findings. JACC Cardiovasc Interv. 2012;5(5):540-551. PMID: 22625193 https://www.jacc.org/doi/abs/10.1016/j.jcin.2012.03.004
Abdel-Wahab M, Mehilli J, Frerker C, et al. Comparison of balloon-expandable vs self-expandable valves in patients undergoing transcatheter aortic valve replacement: the CHOICE randomized clinical trial. JAMA. 2014;311(15):1503-1514. PMID: 24682026. https://jamanetwork.com/journals/jama/fullarticle/1854355
Erkapic D, De Rosa S, Kelava A, Lehmann R, Fichtlscherer S, Hohnloser SH. Risk for permanent pacemaker after transcatheter aortic valve implantation: a comprehensive analysis of the literature. J Cardiovasc Electrophysiol. 2012;23(4):391-397. PMID: 22050112 https://onlinelibrary.wiley.com/doi/10.1111/j.1540-8167.2011.02211.x
Jilaihawi H, Chakravarty T, Weiss RE, Fontana GP, Forrester J, Makkar RR. Me-ta-analysis of complications in aortic valve replacement: comparison of Medtron-ic-Corevalve, Edwards-Sapien and surgical aortic valve replacement in 8,536 patients. Catheter Cardiovasc Interv. 2012;80(1):128-138. PMID: 22415849 https://onlinelibrary.wiley.com/doi/abs/10.1002/ccd.23368
Rodés-Cabau J. Transcatheter aortic valve implantation: current and future approaches. Nat Rev Cardiol. 2011;9(1):15-29. Published 2011 Nov 15. PMDI: 22083020 https://doi.org/10.1038/nrcardio.2011.164
Khatri PJ, Webb JG, Rodés-Cabau J, et al. Adverse effects associated with transcatheter aortic valve implantation: a meta-analysis of contemporary studies. Ann Intern Med. 2013;158(1):35-46. PMID: 23277899 https://www.acpjournals.org/doi/abs/10.7326/0003-4819-158-1-201301010-00007
Nazif TM, Dizon José M, Hahn RT, et al. Predictors and Clinical Outcomes of Perma-nent Pacemaker Implantation After Transcatheter Aortic Valve Replacement. ACC Car-diovasc Interv. 2015;8(1):60-69. PMID: 25616819 https://www.jacc.org/doi/abs/10.1016/j.jcin.2014.07.022
Muñoz-García AJ, Hernández-García JM, Jiménez-Navarro MF, et al. Factors Predict-ing and Having an Impact on the Need for a Permanent Pacemaker After CoreValve Prosthesis Implantation Using the New Accutrak Delivery Catheter System. ACC Car-diovasc Interv. 2012;5(5):533-539. PMID: 22625192 https://www.jacc.org/doi/abs/10.1016/j.jcin.2012.03.011
Ledwoch J, Franke J, Gerckens U, et al. Incidence and predictors of permanent pacemaker implantation following transcatheter aortic valve implantation: analysis from the German transcatheter aortic valve interventions registry. Catheter Cardiovasc Interv. 2013;82(4):E569-E577. PMID: 23475694 https://onlinelibrary.wiley.com/doi/10.1002/ccd.24915
De Carlo M, Giannini C, Bedogni F, et al. Safety of a conservative strategy of permanent pacemaker implantation after transcatheter aortic CoreValve implantation. Am Heart J. 2012;163(3):492-499. PMID: 22424022 https://doi.org/10.1016/j.ahj.2011.12.009
Chorianopoulos E, Krumsdorf U, Pleger ST, Katus HA, Bekeredjian R. Incidence of late occurring bradyarrhythmias after TAVI with the self-expanding CoreValve(®) aortic bioprosthesis. Clin Res Cardiol. 2012;101(5):349-355. PMID: 22179559 https://doi.org/10.1007/s00392-011-0398-9
Bagur R, Manazzoni JM, Dumont É, et al. Permanent pacemaker implantation following isolated aortic valve replacement in a large cohort of elderly patients with severe aortic stenosis. Heart. 2011;97(20):1687-1694. PMID: 21828221 https://heart.bmj.com/content/97/20/1687
Calvi V, Conti S, Pruiti GP, et al. Incidence rate and predictors of permanent pacemaker implantation after transcatheter aortic valve implantation with self-expanding CoreValve prosthesis. J Interv Card Electrophysiol. 2012;34(2):189-195.PMID: 22119855 https://doi.org/10.1007/s10840-011-9634-5
van der Boon RM, Nuis RJ, Van Mieghem NM, et al. New conduction abnormalities after TAVI--frequency and causes. Nat Rev Cardiol. 2012;9(8):454-463. PMID: 22547171 https://doi.org/10.1038/nrcardio.2012.58
Bussink BE, Holst AG, Jespersen L, Deckers JW, Jensen GB, Prescott E. Right bundle branch block: prevalence, risk factors, and outcome in the general population: results from the Copenhagen City Heart Study. Eur Heart J. 2013;34(2):138-146. PMID: 22947613 https://doi.org/10.1093/eurheartj/ehs291
Haataja P, Nikus K, Kähönen M, et al. Prevalence of ventricular conduction blocks in the resting electrocardiogram in a general population: the Health 2000 Survey. Int J Cardiol. 2013;167(5):1953-1960. PMID: 22640691 https://doi.org/10.1016/j.ijcard.2012.05.024
Fischer Q, Himbert D, Webb JG, et al. Impact of Preexisting Left Bundle Branch Block in Transcatheter Aortic Valve Replacement Recipients. Circ Cardiovasc Interv. 2018;11(11):e006927. PMID: 30571207. https://doi.org/10.1161/CIRCINTERVENTIONS.118.006927
Ullah W, Zahid S, Zaidi SR, et al. Predictors of Permanent Pacemaker Implantation in Patients Undergoing Transcatheter Aortic Valve Replacement - A Systematic Review and Meta-Analysis. J Am Heart Assoc. 2021;10(14):e020906. PMID: 34259045 https://doi.org/10.1161/jaha.121.020906
Ravaux JM, Di Mauro M, Vernooy K, et al. Do Women Require Less Permanent Pace-maker After Transcatheter Aortic Valve Implantation? A Meta-Analysis and Me-ta-Regression. J Am Heart Assoc. 2021;10(7):e019429. PMID: 33779244 https://doi.org/10.1161/jaha.120.019429
Buja P, Napodano M, Tamburino C, et al. Comparison of variables in men versus wom-en undergoing transcatheter aortic valve implantation for severe aortic stenosis (from Italian Multicenter CoreValve registry). Am J Cardiol. 2013;111(1):88-93. PMID: 23245837 https://doi.org/10.1016/j.amjcard.2012.08.051.
Spaziano M, Chieffo A, Watanabe Y, et al. Computed tomography predictors of mortality, stroke and conduction disturbances in women undergoing TAVR: A sub-analysis of the WIN-TAVI registry. J Cardiovasc Comput Tomogr. 2018;12(4):338-343. PMID: 29735255 https://doi.org/10.1016/j.jcct.2018.04.007
Ortlepp JR, Pillich M, Schmitz F, et al. Lower serum calcium levels are associated with greater calcium hydroxyapatite deposition in native aortic valves of male patients with severe calcific aortic stenosis. PMID: 16901043.
Aggarwal SR, Clavel MA, Messika-Zeitoun D, et al. Sex differences in aortic valve cal-cification measured by multidetector computed tomography in aortic stenosis. Circ Car-diovasc Imaging. 2013;6(1):40-47. PMID: 23233744 https://doi.org/10.1161/circimaging.112.980052
Petrov G, Regitz-Zagrosek V, Lehmkuhl E, et al. Regression of myocardial hypertrophy after aortic valve replacement: faster in women?. Circulation. 2010;122(11 Suppl):S23-S28. PMID: 20837918 https://doi.org/10.1161/circulationaha.109.927764.
Villari B, Campbell SE, Schneider J, Vassalli G, Chiariello M, Hess OM. Sex-dependent differences in left ventricular function and structure in chronic pressure overload. Eur Heart J. 1995;16(10):1410-1419. PMID: 8746910 https://doi.org/10.1093/oxfordjournals.eurheartj.a060749
Fadahunsi OO, Olowoyeye A, Ukaigwe A, et al. Incidence, Predictors, and Outcomes of Permanent Pacemaker Implantation Following Transcatheter Aortic Valve Replacement: Analysis From the U.S. Society of Thoracic Surgeons/American College of Cardiology TVT Registry. JACC Cardiovasc Interv. 2016;9(21):2189-2199. PMID: 27832844 https://doi.org/10.1016/j.jcin.2016.07.026.
Vernooy K, Verbeek XA, Peschar M, et al. Left bundle branch block induces ventricular remodelling and functional septal hypoperfusion. Eur Heart J. 2005;26(1):91-98. PMID: 15615805 https://doi.org/10.1093/eurheartj/ehi008
Catanzariti D, Maines M, Manica A, Angheben C, Varbaro A, Vergara G. Permanent His-bundle pacing maintains long-term ventricular synchrony and left ventricular per-formance, unlike conventional right ventricular apical pacing. Europace. 2013;15(4):546-553. PMID: 22997222 https://doi.org/10.1093/europace/eus313.
Barold SS, Ovsyshcher IE. Pacemaker-induced mitral regurgitation. Pacing Clin Elec-trophysiol. 2005;28(5):357-360. PMID: 15869664 https://doi.org/10.1111/j.1540-8159.2005.09486.x
Kaplan RM, Yadlapati A, Cantey EP, et al. Conduction recovery following pacemaker implantation after transcatheter aortic valve replacement. Pacing Clin Electrophysiol. 2019;42(2):146-152. PMID: 30548869 https://doi.org/10.1111/pace.13579.
European Society of Cardiology (ESC); European Heart Rhythm Association (EHRA), Brignole M, et al. 2013 ESC guidelines on cardiac pacing and cardiac resynchronization therapy: the task force on cardiac pacing and resynchronization therapy of the European Society of Cardiology (ESC). Developed in collaboration with the European Heart Rhythm Association (EHRA). Europace. 2013;15(8):1070-1118. PMID: 23801827. https://doi.org/10.1093/eurheartj/eht150
Lilly SM, Deshmukh AJ, Epstein AE, et al. 2020 ACC Expert Consensus Decision Pathway on Management of Conduction Disturbances in Patients Undergoing Transcatheter Aortic Valve Replacement: A Report of the American College of Cardiology Solution Set Oversight Committee. J Am Coll Cardiol. 2020;76(20):2391-2411. PMID: 33190683 https://doi.org/0.1016/j.jacc.2020.08.050
Krishnaswamy A, Sammour Y, Mangieri A, et al. The Utility of Rapid Atrial Pacing Immediately Post-TAVR to Predict the Need for Pacemaker Implantation. JACC Cardiovasc Interv. 2020;13(9):1046-1054. PMID: 32305392 https://doi.org/10.1016/j.jcin.2020.01.215
Ahmad M, Patel JN, Loc BL, et al. Permanent Pacemaker Implantation After Transcatheter Aortic Valve Replacement: A Cost Analysis. Cureus. 2019;11(6):e5005. PMID: 31281768. https://doi.org/10.7759/cureus.5005
Published
How to Cite
Issue
Section
Copyright (c) 2022 International Journal of Clinical Research

This work is licensed under a Creative Commons Attribution 4.0 International License.