A Case of an Adult Complicated Left Diaphragmatic Hernia: Case Report and Literature Review
DOI:
https://doi.org/10.38179/ijcr.v4i1.235Keywords:
Case report, Diaphragmatic hernia, Iatrogenic diaphragmatic hernia, Left nephrectomy, SplenectomyAbstract
Introduction: Diaphragmatic hernia by definition is the protrusion of abdominal structures into the thoracic cavity. Classified as either congenital or acquired, adult diaphragmatic hernia without a history of trauma is rare, and iatrogenic diaphragmatic hernia is rarer. The array of symptoms may be acute or latent and will depend on the herniated organ, which certainly makes this pathology a challenge at the level of diagnosis and subsequent management.
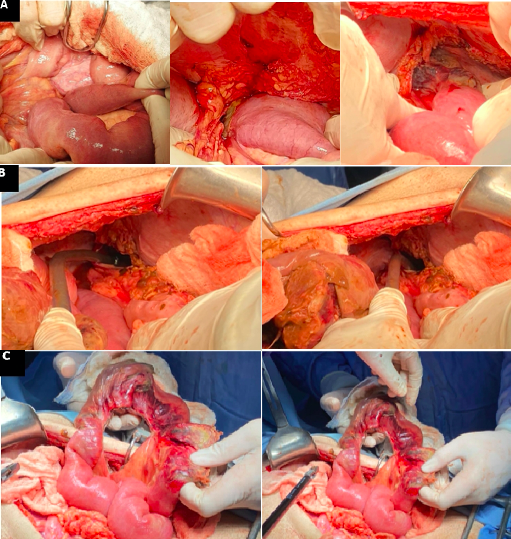
Case Report: Here we present the case of a 73-year-old male patient who presented one year post left nephrectomy complicated by splenectomy (post splenic injury), with two weeks history of diffuse abdominal pain, non-bilious vomiting, and shortness of breath. Workup done revealed a left diaphragmatic hernia containing necrotic-perforated small bowel loops. A laparotomy with intestinal resection, loop ileostomy along with a primary repair of the diaphragmatic defect were performed.
Conclusion: Although a great portion of acquired diaphragmatic hernias remain asymptomatic, they may be presenting with severe symptomatology and aggravating complications. At the level of clinical manifestation, suspicion of diaphragmatic hernia ascends the ladder of differential diagnosis in a patient with combined respiratory and gastrointestinal symptoms and hence is essential to avoid delayed treatment and superimposing lethal complications. Definitive treatment of diaphragmatic hernia is surgical repair given the high morbidity and mortality associated with such injury.
References
Spellar K, Lotfollahzadeh S, Gupta N. Diaphragmatic Hernia. In: StatPearls. Treasure Island (FL): StatPearls Publishing; August 21, 2023. PMID: 30725637
Mínguez Ruiz G, García Florez LJ, Arias Pacheco RD, García Bear I, Ramos Pérez V, Pire Abaitua G. Post-nephrectomy diaphragmatic hernia. Increase suspicion and decrease morbi-mortality: two cases report. J Surg Case Rep. 2018;2018(8):rjy224. Published 2018 Aug 20. doi:10.1093/jscr/rjy224. PMID: 30151114. https://doi.org/10.1093%2Fjscr%2Frjy224
Lu J, Wang B, Che X, et al. Delayed traumatic diaphragmatic hernia: A case-series report and literature review. Medicine (Baltimore). 2016;95(32):e4362. PMID: 27512848. https://doi.org/10.1097/md.0000000000004362
Postnephrectomy diaphragmatic hernia presenting as progressive dyspnoea, Azam A, Michael K. BMJ Case Rep 2020. PMID: 27512848
Ye D, Hu Y, Zhu N, et al. Exploratory Investigation of Intestinal Structure and Function after Stroke in Mice. Mediators Inflamm. 2021;2021:1315797. Published 2021 Feb 15. PMID: 33642941. https://doi.org/10.1155/2021/1315797
Schaller BJ, Graf R, Jacobs AH. Pathophysiological changes of the gastrointestinal tract in ischemic stroke. Am J Gastroenterol. 2006;101(7):1655-1665. PMID: 16863574. https://doi.org/10.1111/j.1572-0241.2006.00540.x
Huda T, Pandya B. Jejunal obstruction due to ischemic stricture: An unusual presentation. International Surgery Journal. http://dx.doi.org/10.18203/2349-2902.isj20190378.
Koshikawa Y, Nakase H, Matsuura M, et al. Ischemic enteritis with intestinal stenosis. Intest Res. 2016;14(1):89-95. PMID: 26884740. https://doi.org/10.5217%2Fir.2016.14.1.89
Takeuchi N, Naba K. Small intestinal obstruction resulting from ischemic enteritis: a case report. Clin J Gastroenterol. 2013;6(4):281-286. PMID: 23990850. https://doi.org/10.1007/s12328-013-0393-y
Gonzalez AJ, Afraz S, Melendez-Rosado J, Schneider A. Isolated Jejunal Crohn's Disease Masquerading as Gastroparesis. Cureus. 2022;14(6):e26333. Published 2022 Jun 25. PMID: 35775060.
https://doi.org/10.7759/cureus.26333
Kishore GS, Gupta V, Doley RP, et al. Traumatic diaphragmatic hernia: tertiary centre experience. Hernia. 2010;14(2):159-164. PMID: 19908108. https://doi.org/10.1007/s10029-009-0579-x
Matthews BD, Bui H, Harold KL, et al. Laparoscopic repair of traumatic diaphragmatic injuries. Surg Endosc. 2003;17(2):254-258. PMID: 12399834. https://doi.org/10.1007/s00464-002-8831-9
Gulamhusein, T., Obeid, N.R., Pryor, A.D. Surgical Management: Other Diaphragmatic Hernias in Adults. The SAGES Manual of Foregut Surgery. Springer, Cham. 2019 https://doi.org/10.1007/978-3-319-96122-4_23
Published
How to Cite
Issue
Section
Copyright (c) 2024 International Journal of Clinical Research

This work is licensed under a Creative Commons Attribution 4.0 International License.







