The First Reported Case of Pulmonary Embolism and Deep Vein Thrombosis Associated with Intraductal Papillary Mucinous Neoplasm: A Case Report
DOI:
https://doi.org/10.38179/ijcr.v3i1.247Keywords:
Intraductal papillary mucinous neoplasm, Deep vein thrombosis, Pulmonary embolism, Pancreas, CancerAbstract
Background: Reported cases of Intraductal papillary mucinous neoplasm (IPMN) are becoming more and more frequent. The risk of hypercoagulability associated with IPMN is not clearly established in the literature as it was only reported in four cases. Therefore, we present a unique case of a patient with IPMN who subsequently developed acute pulmonary embolism (PE) and deep venous thrombosis (DVT).
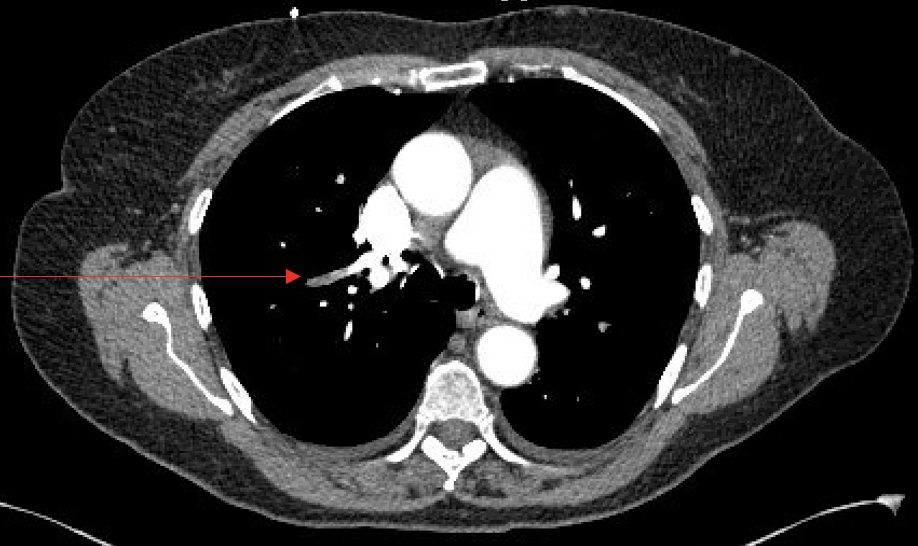
Case presentation: A 70-year-old healthy female patient complained of palpitation, chest pain, and dyspnea at rest. She had normal vital signs and findings on physical examination. Laboratory tests showed an increase in the D-Dimer level of 3,730 ng/mL fibrinogen equivalent unit (FEU). Bilateral DVT ultrasound (DVT-US) of the lower extremities was positive for acute calf DVT in the right lower extremity involving the soleal vein. CT-PE chest with IV contrast was remarkable for segmental and subsegmental pulmonary arteries thrombosis. She was started on a heparin drip and then transitioned to rivaroxaban for the treatment of PE and DVT. She was discharged in stable condition with outpatient follow-up.
Conclusion: IPMN of the pancreas is an exocrine pancreatic neoplasm often detected on Computed Tomography (CT) scan or Magnetic Resonance Imaging (MRI). It is usually non-malignant but was found to be more prone to progress into cancer in contrast to the other types of pancreatic cysts. An increased risk of hypercoagulability with pre-malignant pancreatic lesions such as IPMN has not yet been well established. As far as we know, this case report is the first article presenting IPMN associated with both acute DVT and PE in a relatively healthy individual with no prior risk factor for hypercoagulability. Although there is scattered evidence suggesting an increased risk of thromboembolic events with IPMN, this unique case of DVT and PE associated with IPMN highlights the importance of close monitoring of these patients, especially those who have risk factors for thrombosis.
References
Tanaka M. Clinical Management and Surgical Decision-Making of IPMN of the Pancreas. Methods Mol Biol. 2019;1882:9-22. PMID: 30378040. https://doi.org/10.1007/978-1-4939-8879-2_2
Machado NO, Al Qadhi H, Al Wahibi K. Intraductal Papillary Mucinous Neoplasm of Pancreas. N Am J Med Sci. 2015;7(5):160-175. PMID: 26110127. https://doi.org/10.4103%2F1947-2714.157477
Khan S, Sclabas G, Reid-Lombardo KM. Population-based epidemiology, risk factors and screening of intraductal papillary mucinous neoplasm patients. World J Gastrointest Surg. 2010;2(10):314-318. PMID: 21160836. https://doi.org/10.4240/wjgs.v2.i10.314
Yoon JG, Smith D, Ojili V, Paspulati RM, Ramaiya NH, Tirumani SH. Pancreatic cystic neoplasms: a review of current recommendations for surveillance and management. Abdom Radiol (NY). 2021;46(8):3946-3962. PMID: 33742217. https://doi.org/10.1007/s00261-021-03030-x
Oyama H, Tada M, Takagi K, et al. Long-term Risk of Malignancy in Branch-Duct Intraductal Papillary Mucinous Neoplasms. Gastroenterology. 2020;158(1):226-237.e5. PMID: 31473224. https://doi.org/10.1053/j.gastro.2019.08.032
Adsay V, Mino-Kenudson M, Furukawa T, et al. Pathologic Evaluation and Reporting of Intraductal Papillary Mucinous Neoplasms of the Pancreas and Other Tumoral Intraepithelial Neoplasms of Pancreatobiliary Tract: Recommendations of Verona Consensus Meeting. Ann Surg. 2016;263(1):162-177. PMID: 25775066. https://doi.org/10.1097/sla.0000000000001173
Basturk O, Hong SM, Wood LD, et al. A Revised Classification System and Recommendations From the Baltimore Consensus Meeting for Neoplastic Precursor Lesions in the Pancreas. Am J Surg Pathol. 2015;39(12):1730-1741. PMID: 26559377. https://doi.org/10.1097/pas.0000000000000533
Hruban RH, Takaori K, Klimstra DS, et al. An illustrated consensus on the classification of pancreatic intraepithelial neoplasia and intraductal papillary mucinous neoplasms. Am J Surg Pathol. 2004;28(8):977-987. PMID: 15252303. https://doi.org/10.1097/01.pas.0000126675.59108.80
Hecht EM, Khatri G, Morgan D, et al. Intraductal papillary mucinous neoplasm (IPMN) of the pancreas: recommendations for Standardized Imaging and Reporting from the Society of Abdominal Radiology IPMN disease focused panel. Abdom Radiol (NY). 2021;46(4):1586-1606. PMID: 33185741. https://doi.org/10.1007/s00261-020-02853-4
Abdol Razak NB, Jones G, Bhandari M, Berndt MC, Metharom P. Cancer-Associated Thrombosis: An Overview of Mechanisms, Risk Factors, and Treatment. Cancers (Basel). 2018;10(10):380. PMID: 30314362. https://doi.org/10.3390%2Fcancers10100380
Sheth RA, Niekamp A, Quencer KB, et al. Thrombosis in cancer patients: etiology, incidence, and management. Cardiovasc Diagn Ther. 2017;7(Suppl 3):S178-S185. PMID: 29399521. https://doi.org/10.21037%2Fcdt.2017.11.02
Samare Fekri M, Khalily Zade M, Fatehi S. The association of deep vein thrombosis with cancer treatment modality: chemotherapy or surgery?. Iran Red Crescent Med J. 2014;16(9):e14722. PMID: 25593718. https://doi.org/10.5812%2Fircmj.14722
Asanuma K, Nakamura T, Okamoto T, et al. Do coagulation or fibrinolysis reflect the disease condition in patients with soft tissue sarcoma?. BMC Cancer. 2022;22(1):1075. PMID: 36258189. https://doi.org/10.1186%2Fs12885-022-10106-4
Cherif Y, Ghariani R, Mrouki M, et al. Deep Venous Thrombosis and Intraductal Papillary and Mucinous Tumor of the Pancreas: about 3 Cases [abstract]. Res Pract Thromb Haemost. 2020; 4 (Suppl 1). https://abstracts.isth.org/abstract/deep-venous-thrombosis-and-intraductal-papillary-and-mucinous-tumor-of-the-pancreas-about-3-cases/.
Sweetser S, Vege SS, Clain JE, Topazian MD. Does splenic vein thrombosis predict invasive malignancy in side-branch intraductal papillary mucinous neoplasm (IPMN)?. Am J Gastroenterol. 2008;103(9):2412-2413. PMID: 18844637. https://doi.org/10.1111/j.1572-0241.2008.02010_12.x
Bhosale P, Balachandran A, Tamm E. Imaging of benign and malignant cystic pancreatic lesions and a strategy for follow up. World J Radiol. 2010;2(9):345-353. PMID: 21160696. https://doi.org/10.4329%2Fwjr.v2.i9.345
Farrell JJ. Pancreatic Cysts and Guidelines. Dig Dis Sci. 2017;62(7):1827-1839. https://doi.org/10.1007/s10620-017-4571-5
Govsyeyev N, Malgor RD, Hoffman C, et al. A systematic review and meta-analysis of outcomes after acute limb ischemia in patients with cancer. J Vasc Surg. 2021;74(3):1033-1040.e1. https://doi.org/10.1016/j.jvs.2021.03.058
Hicks AM, DeRosa A, Raj M, et al. Visceral Thromboses in Pancreas Adenocarcinoma: Systematic Review. Clin Colorectal Cancer. 2018;17(2):e207-e216. PMID: 29306522. https://doi.org/10.1016%2Fj.clcc.2017.12.001
Published
How to Cite
Issue
Section
Copyright (c) 2022 International Journal of Clinical Research

This work is licensed under a Creative Commons Attribution 4.0 International License.







