Uveitis as a Manifestation of Celiac Disease: A Population-Based Study
DOI:
https://doi.org/10.38179/ijcr.v3i1.250Keywords:
Autoimmune disease, Celiac disease, UveitisAbstract
Introduction: The prevalence of celiac disease (CD) in the United States population has been estimated to be 0.71%, or 1 in 141, with the prevalence in first- and second-degree relatives of those affected being 4.55% and 2.59% respectively. Due to the multitude of ways in which this disease may initially present, it is important to screen for CD to avoid the potential consequences of inadequately managed disease. Many ophthalmic conditions have also been implicated as extraintestinal manifestations of CD, including uveitis. Despite several studies and case reports suggesting a positive correlation between CD and uveitis, there has yet to be a nationwide study in the United States quantifying this relationship. Therefore, the aim of this study is to conduct a large-scale multi-center population-based study to assess whether there is a statistically significant increased risk of uveitis in individuals with celiac disease.
Methods: A validated multicenter and research platform database of more than 360 hospitals from 26 different healthcare systems across the United States consisting of data accumulated from 1999 to September 2022 was utilized to construct this study. We excluded patients with a history of autoimmune diseases, cataract surgery, or any type of eye infection. We included a subgroup of patients with a diagnosis of “uveitis” for further analysis. The risk of developing uveitis was calculated using a univariate logistic regression. A multivariate analysis was also done to account for confounding variables including African American ethnicity, male gender, sexually transmitted diseases, and celiac disease.
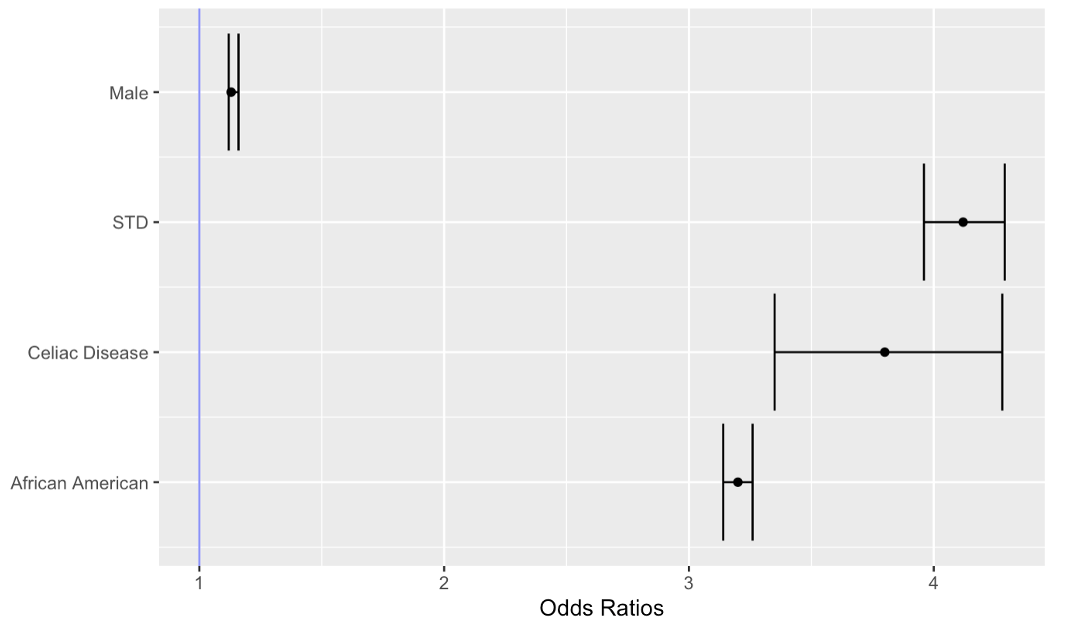
Results: 70,632,440 patients were screened and a cohort of 46,895,750 individuals was selected for the final analysis after accounting for inclusion and exclusion criteria were met. The incidence of uveitis in patients with celiac disease in the past 3 years was 280 per 100,000 people. The prevalence of uveitis in the US population from 1999 to September 2022 was 150 per 100,000 people (0.15%). In order to adjust for confounding variables, a multivariate regression analysis was performed and showed an increased risk of being African-American (OR: 3.20%; 95% CI: 3.14-3.26) and male (OR: 1.13%; 95% CI: 1.12-1.16); and having a diagnosis of celiac disease (OR: 3.80%; 95% CI: 3.35-4.28) and sexually transmitted diseases (OR: 4.12%; 95% CI: 3.96-4.29) in patients with uveitis.
Discussion: Recent population-based studies demonstrated that the prevalence of CD in the United States is much greater than previously thought, such that a trend of underdiagnoses is suspected to have occurred for several years. Many newly diagnosed uveitis cases, 48%, have been classified as idiopathic uveitis even after a complete workup was done. Several studies have been published in which a correlation between uveitis and CD is reported. The findings of this study further emphasize the importance of a thorough workup to evaluate for an underlying inflammatory process prior to diagnosing uveitis as idiopathic.
Conclusion: In conclusion, we established that patients with celiac disease are at increased risk of developing uveitis after excluding and controlling for any confounding variables. In further studies, it could be interesting to investigate the impact of gluten-free diet in patients with celiac disease on the risk of developing uveitis.
References
Rubio-Tapia A, Ludvigsson JF, Brantner TL, Murray JA, Everhart JE. The prevalence of celiac disease in the United States. Am J Gastroenterol. 2012 Oct;107(10):1538-44; quiz 1537, 1545. https://doi.org/10.1038/ajg.2012.219 . Epub 2012 Jul 31. PMID: 22850429.
Fasano A, Berti I, Gerarduzzi T, Not T, Colletti RB, Drago S, Elitsur Y, Green PH, Guandalini S, Hill ID, Pietzak M, Ventura A, Thorpe M, Kryszak D, Fornaroli F, Wasserman SS, Murray JA, Horvath K. Prevalence of celiac disease in at-risk and not-at-risk groups in the United States: a large multicenter study. Arch Intern Med. 2003 Feb 10;163(3):286-92. https://doi.org/10.1038%2Fajg.2011.21 . PMID: 12578508.
Celiac disease u.s. department of health and human services national institutes of health https://permanent.fdlp.gov/gpo12733/celiac.pdf
Gritz DC, Wong IG. Incidence and prevalence of uveitis in Northern California; the Northern California Epidemiology of Uveitis Study. Ophthalmology. 2004 Mar;111(3):491-500; discussion 500. https://doi.org/10.1016/j.ophtha.2003.06.014 . PMID: 15019324.
Suhler EB, Lloyd MJ, Choi D, Rosenbaum JT, Austin DF. Incidence and prevalence of uveitis in Veterans Affairs Medical Centers of the Pacific Northwest. Am J Ophthalmol. 2008 Dec;146(6):890-6.e8. https://doi.org/10.1016/j.ajo.2008.09.014 . PMID: 19027424.
Acharya NR, Tham VM, Esterberg E, Borkar DS, Parker JV, Vinoya AC, Uchida A. Incidence and prevalence of uveitis: results from the Pacific Ocular Inflammation Study. JAMA Ophthalmol. 2013 Nov;131(11):1405-12 https://doi.org/10.1001/jamaophthalmol.2013.4237 . PMID: 24008391.
IBM Corporation. The IBM Explorys Platform: liberate your healthcare data. Available online: https://www.ibm.com/downloads/cas/4P0QB9JN . Last accessed Novemeber 28, 2020. :5.
US National Library of Medicine Unified Medical Language System (UMLS). Systematized Nomenclature of Medicine– Clinical Terms (SNOMED CT). https://www.nlm.nih.gov/research/umls/Snomed/snomed_main.html .
Nelson SJ, Zeng K, Kilbourne J, Powell T, Moore R. Normalized names for clinical drugs: RxNorm at 6 years. J. Am. Med. Inform. Assoc. 2011; 18: 441–8.
Mollazadegan K, Kugelberg M, Tallstedt L, Ludvigsson JF. Increased risk of uveitis in coeliac disease: a nationwide cohort study. Br J Ophthalmol. 2012 Jun;96(6):857-61. https://doi.org/10.1136/bjophthalmol-2011-301051 . Epub 2012 Mar 9. PMID: 22408231.
Klack K, Pereira RM, de Carvalho JF. Uveitis in celiac disease with an excellent response to gluten-free diet: third case described. Rheumatol Int. 2011 Mar;31(3):399-402. https://doi.org/10.1007/s00296-009-1177-z . Epub 2009 Oct 14. PMID: 19826819.
Huang XF, Brown MA. Progress in the genetics of uveitis. Genes Immun. 2022 Apr;23(2):57-65. https://doi.org/10.1038%2Fs41435-022-00168-6 . Epub 2022 Apr 4. PMID: 35379982
Brown NK, Guandalini S, Semrad C, Kupfer SS. A Clinician's Guide to Celiac Disease HLA Genetics. Am J Gastroenterol. 2019 Oct;114(10):1587-1592. https://doi.org/10.14309/ajg.0000000000000310 . PMID: 31274511.
Alshiekh S, Geraghty DE, Agardh D. High-resolution genotyping of HLA class I loci in children with type 1 diabetes and celiac disease. HLA. 2021 Jun;97(6):505-511. https://doi.org/10.1111/tan.14280 . Epub 2021 May 4. PMID: 33885207.
Goel G, Tye-Din JA, Qiao SW, Russell AK, Mayassi T, Ciszewski C, Sarna VK, Wang S, Goldstein KE, Dzuris JL, Williams LJ, Xavier RJ, Lundin KEA, Jabri B, Sollid LM, Anderson RP. Cytokine release and gastrointestinal symptoms after gluten challenge in celiac disease. Sci Adv. 2019 Aug 7;5(8):eaaw7756. https://doi.org/10.1126/sciadv.aaw7756 . PMID: 31457091
Abadie V, Kim SM, Lejeune T, Palanski BA, Ernest JD, Tastet O, Voisine J, Discepolo V, Marietta EV, Hawash MBF, Ciszewski C, Bouziat R, Panigrahi K, Horwath I, Zurenski MA, Lawrence I, Dumaine A, Yotova V, Grenier JC, Murray JA, Khosla C, Barreiro LB, Jabri B. IL-15, gluten and HLA-DQ8 drive tissue destruction in coeliac disease. Nature. 2020 Feb;578(7796):600-604. https://doi.org/10.1038/s41586-020-2003-8 . Epub 2020 Feb 12. PMID: 32051586
Errera MH, Pratas A, Fisson S, Manicom T, Boubaya M, Sedira N, Héron E, Merabet L, Kobal A, Levy V, Warnet JM, Chaumeil C, Brignole-Baudouin F, Sahel JA, Goldschmidt P, Bodaghi B, Bloch-Queyrat C. Cytokines, chemokines and growth factors profile in human aqueous humor in idiopathic uveitis. PLoS One. 2022 Jan 21;17(1):e0254972. https://doi.org/10.1371/journal.pone.0254972 . PMID: 35061677
Alkhayyat M. Epidemiology of neuroendocrine tumors of the appendix in the USA: a population-based national study (2014-2019). Ann Gastroenterol. Published online 2021. https://doi.org/10.20524%2Faog.2021.0643
Alkhayyat M, Qapaja T, Aggarwal M, et al. Epidemiology and risk of psychiatric disorders among patients with celiac disease: A population‐based national study. J Gastroenterol Hepatol. 2021;36(8):2165-2170. https://doi.org/10.1111/jgh.15437
Kubihal S, Gupta Y, Shalimar, et al. Prevalence of non‐alcoholic fatty liver disease and factors associated with it in Indian women with a history of gestational diabetes mellitus. J Diabetes Investig. 2021;12(5):877-885. https://doi.org/10.1111/jdi.13411
Published
How to Cite
Issue
Section
Copyright (c) 2022 International Journal of Clinical Research

This work is licensed under a Creative Commons Attribution 4.0 International License.







