SARS, MERS, COVID-19: Identification of Patients at a Higher Risk: A Narrative Review
DOI:
https://doi.org/10.38179/ijcr.v2i1.47Keywords:
SARS-CoV, MERS-CoV, SARS-CoV-2, COVID-19, Cardiovascular disease, Hypertension, Immune suppression, High-risk, Pregnancy, Risk factorsAbstract
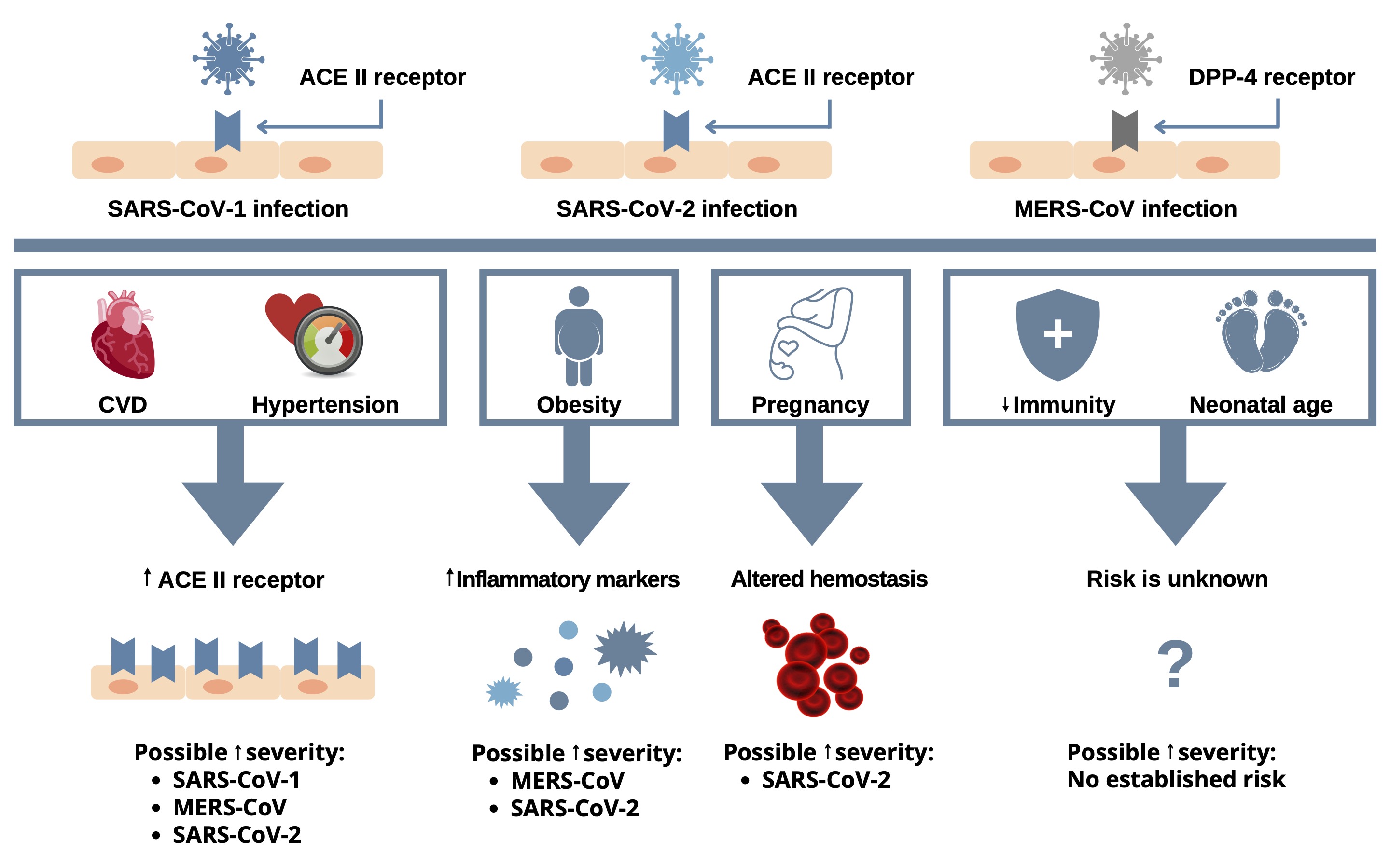
The different presentations, comorbidities, and outcomes of COVID-19 highlight the importance of early identification and proper triage of patients. High-risk patients can be divided into patients with common comorbidities and patients with special categories. Common comorbidities include, but are not limited to, Cardiovascular Disease (CVD), Diabetes Mellitus (DM), immunosuppression, underlying respiratory disease, and obesity. Certain categories of COVID-19 patients are also at increased risk, including neonates and pregnant women. In the present article, we delineate the reported risk factors for acquisition of infection, and for increased severity of the clinical disease. We also comparatively analyze those risk factors associated with COVID-19 and with the antecedent human acute respiratory syndrome-causing viruses, SARS-CoV-1 and MERS-CoV. We hypothesize that the structural similarities of the three viruses predict a similarity in the profile of high-risk patients. Several pathophysiological patterns have been detected to support this theory.
References
World Health Organization. WHO Coronavirus Disease (COVID-19) Dashboard. 2020, December 1.
World Health Organization. Summary of probable SARS cases with onset of illness from 1 November 2002 to 31 July 2003. 2015, July 24.
World Health Organization. Middle East respiratory syndrome coronavirus (MERS-CoV) - The Kingdom of Saudi Arabia. 2020, February 2020.
Turner A, Hiscox J and Hooper N. ACE2: from vasopeptidase to SARS virus receptor. Trends Pharmacol Sci. 2004; 25: 291-4. https://doi.org/10.1016/j.tips.2004.04.001
Müller MA, Raj VS, Muth D, et al. Human coronavirus EMC does not require the SARS-coronavirus receptor and maintains broad replicative capability in mammalian cell lines. MBio. 2012; 3: e00515-12. https://doi.org/10.1128/mBio.00515-12
Raj VS, Mou H, Smits SL, et al. Dipeptidyl peptidase 4 is a functional receptor for the emerging human coronavirus-EMC. Nature. 2013; 495: 251-4. https://doi.org/10.1038/nature12005
Zheng Y-Y, Ma Y-T, Zhang J-Y and Xie X. COVID-19 and the cardiovascular system. Nat Rev Cardiol. 2020: 1-2. https://doi.org/10.1038/s41569-020-0360-5
Sakabe M, Yoshioka R and Fujiki A. Sick sinus syndrome induced by interferon and ribavirin therapy in a patient with chronic hepatitis C. J Cardiol Cases. 2013; 8: 173-5. https://doi.org/10.1016/j.jccase.2013.08.002
Wang D, Hu B, Hu C, et al. Clinical Characteristics of 138 Hospitalized Patients With 2019 Novel Coronavirus-Infected Pneumonia in Wuhan, China. JAMA. 2020; 323: 1061-9. https://doi.org/10.1001/jama.2020.1585
Zhang J, Dong X, Cao Y, et al. Clinical characteristics of 140 patients infected with SARS-CoV-2 in Wuhan, China. Allergy. 2020; 00: 1-12. https://doi.org/10.1111/all.14238
Yang X, Yu Y, Xu J, et al. Clinical course and outcomes of critically ill patients with SARS-CoV-2 pneumonia in Wuhan, China: a single-centered, retrospective, observational study. The Lancet Respiratory Medicine. 2020; 8: 475-81. https://doi.org/10.1016/S2213-2600(20)30079-5
Zhou F, Yu T, Du R, et al. Clinical course and risk factors for mortality of adult inpatients with COVID-19 in Wuhan, China: a retrospective cohort study. The Lancet. 2020; 395: 1054-62. https://doi.org/10.1016/S0140-6736(20)30566-3
Lambeir A, Durinx C, Scharpé S and De IM. Dipeptidyl-peptidase IV from bench to bedside: an update on structural properties, functions, and clinical aspects of the enzyme DPP IV. Crit Rev Clin Lab Sci. 2003; 40: 209-94. https://doi.org/10.1080/713609354
Hamming I, Cooper M, Haagmans B, et al. The emerging role of ACE2 in physiology and disease. J Pathol. 2007; 212: 1-11. https://doi.org/10.1002/path.2162
Wan Y, Shang J, Graham R, Baric R and Li F. Receptor Recognition by the Novel Coronavirus from Wuhan: an Analysis Based on Decade-Long Structural Studies of SARS Coronavirus. J Virol. 2020; 94: e00127-20. https://doi.org/10.1128/JVI.00127-20
Zhang P, Zhu L, Cai J, et al. Association of inpatient use of angiotensin converting enzyme inhibitors and angiotensin II receptor blockers with mortality among patients with hypertension hospitalized with COVID-19. Circ Res. 2020; 126: 1671-81. https://doi.org/10.1161/CIRCRESAHA.120.317134
Huang C, Wang Y, Li X, et al. Clinical features of patients infected with 2019 novel coronavirus in Wuhan, China. Lancet. 2020; 395: 497-506. https://doi.org/10.1016/S0140-6736(20)30183-5
Li B, Yang J, Zhao F, et al. Prevalence and impact of cardiovascular metabolic diseases on COVID-19 in China. Clin Res Cardiol. 2020; 109: 531-8. https://doi.org/10.1007/s00392-020-01626-9
Mehra MR, Desai SS, Kuy S, Henry TD and Patel AN. Cardiovascular disease, drug therapy, and mortality in Covid-19. N Engl J Med. 2020; 382: e102. https://doi.org/10.1056/NEJMoa2007621
Ng TM and Toews ML. Impaired norepinephrine regulation of monocyte inflammatory cytokine balance in heart failure. World J Cardiol. 2016; 8: 584. https://doi.org/10.4330/wjc.v8.i10.584
Wang D, Hu B, Hu C, et al. Clinical Characteristics of 138 Hospitalized Patients With 2019 Novel Coronavirus-Infected Pneumonia in Wuhan, China. JAMA. 2020. https://doi.org/10.1001/jama.2020.1585
Al Zaghrini E, Emmanuel N, Zibara V, Terro WD, Hanna S. COVID-19 Myocarditis Clinical Presentation, Diagnosis and Management: A Narrative Review. Int J Clin Res. 2021. 135-50. https://doi.org/10.38179/ijcr.v1i1.27
Heymans S. Myocarditis and heart failure: need for better diagnostic, predictive, and therapeutic tools. Eur Heart J. 2007; 28: 1279-80. https://doi.org/10.1093/eurheartj/ehm111
Alhogbani T. Acute myocarditis associated with novel Middle east respiratory syndrome coronavirus. Ann Saudi Med. 2016; 36: 78-80. https://doi.org/10.5144/0256-4947.2016.78
Arabi Y, Arifi A, Balkhy H, et al. Clinical course and outcomes of critically ill patients with Middle East respiratory syndrome coronavirus infection. Ann Intern Med. 2014; 160: 389-97. https://doi.org/10.7326/M13-2486
Alsolamy S. Middle East respiratory syndrome: knowledge to date. Crit Care Med. 2015; 43: 1283-90. https://doi.org/10.1097/CCM.0000000000000966
Al-Tawfiq J, Hinedi K, Ghandour J, et al. Middle East respiratory syndrome coronavirus: a case-control study of hospitalized patients. Clin Infect Dis. 2014; 59: 160-5. https://doi.org/10.1093/cid/ciu226
Badawi A and Ryoo S. Prevalence of comorbidities in the Middle East respiratory syndrome coronavirus (MERS-CoV): a systematic review and meta-analysis. Int J Infect Dis. 2016; 49: 129-33. https://doi.org/10.1016/j.ijid.2016.06.015
Zhonghua Shao Shang Za ZhiZhonghua zhong liu za zhi [Chinese journal of oncology]Ansari MA, Marchi E, Ramamurthy N, et al. Negative regulation of ACE2 by interferons in vivo and its genetic control. medRxiv. 2020.
Wu Q, Zhou L, Sun X, et al. Altered Lipid Metabolism in Recovered SARS Patients Twelve Years after Infection. Sci Rep. 2017; 7: 9110-. https://doi.org/10.1038/s41598-017-09536-z
Kamboj M and Sepkowitz K. Nosocomial infections in patients with cancer. Lancet Oncol. 2009; 10: 589-97. https://doi.org/10.1016/S1470-2045(09)70069-5
Li J, Duan X, Wang L, et al. Selective depletion of regulatory T cell subsets by docetaxel treatment in patients with nonsmall cell lung cancer. J Immunol Res. 2014; 2014: 286170-. https://doi.org/10.1155/2014/286170
Longbottom E, Torrance H, Owen H, et al. Features of Postoperative Immune Suppression Are Reversible With Interferon Gamma and Independent of Interleukin-6 Pathways. ann surg. 2016; 264: 370-7. https://doi.org/10.1097/SLA.0000000000001484
Sica A and Massarotti M. Myeloid suppressor cells in cancer and autoimmunity. J Autoimmun. 2017; 85: 117-25. https://doi.org/10.1016/j.jaut.2017.07.010
Hilgenfeld R and Peiris M. From SARS to MERS: 10 years of research on highly pathogenic human coronaviruses. Antiviral Res. 2013; 100: 286-95. https://doi.org/10.1016/j.antiviral.2013.08.015
Jiang S and Shi Z. The First Disease X is Caused by a Highly Transmissible Acute Respiratory Syndrome Coronavirus. Virol Sin. 2020. https://doi.org/10.1007/s12250-020-00206-5
D'Antiga L. Coronaviruses and immunosuppressed patients. The facts during the third epidemic. Liver Transpl. 2020. https://doi.org/10.1002/lt.25756
Hui D, Azhar E, Kim Y, Memish Z, Oh M and Zumla A. Middle East respiratory syndrome coronavirus: risk factors and determinants of primary, household, and nosocomial transmission. Lancet Infect Dis. 2018; 18: e217-e27. https://doi.org/10.1016/S1473-3099(18)30127-0
Liang W, Guan W, Chen R, et al. Cancer patients in SARS-CoV-2 infection: a nationwide analysis in China. Lancet Oncol. 2020; 21: 335-7. https://doi.org/10.1016/S1470-2045(20)30096-6
Zheng R, Sun K, Zhang S, et al. Report of cancer epidemiology in China, 2015. Chin J Oncol. 2019; 41: 19-28.
Gosain R, Abdou Y, Singh A, Rana N, Puzanov I and Ernstoff M. COVID-19 and Cancer: a Comprehensive Review. Curr Oncol Rep. 2020; 22: 53. https://doi.org/10.1007/s11912-020-00934-7
Stockman L, Massoudi M, Helfand R, et al. Severe acute respiratory syndrome in children. Pediatr Infect Dis J. 2007; 26: 68-74. https://doi.org/10.1097/01.inf.0000247136.28950.41
Mandl J, Schneider C, Schneider D and Baker M. Going to Bat (s) for Studies of Disease Tolerance. Front Immunol. 2018; 9: 2112-. https://doi.org/10.3389/fimmu.2018.02112
Mandl J, Ahmed R, Barreiro L, et al. Reservoir host immune responses to emerging zoonotic viruses. Cell. 2015; 160: 20-35. https://doi.org/10.1016/j.cell.2014.12.003
Wang H and Zhang L. Risk of COVID-19 for patients with cancer. Lancet Oncol. 2020; 21: e181. https://doi.org/10.1016/S1470-2045(20)30149-2
Centers for Disease Control and Prevention (CDC). People Who Are at Higher Risk for Severe Illness. 2020, April 2.
Dietz W and Santos-Burgoa C. Obesity and its Implications for COVID-19 Mortality. Obesity (Silver Spring). 2020; 28. https://doi.org/10.1002/oby.22818
Simonnet A, Chetboun M, Poissy J, et al. High prevalence of obesity in severe acute respiratory syndrome coronavirus‐2 (SARS‐CoV‐2) requiring invasive mechanical ventilation. Obesity. 2020; 28: 1195-9. https://doi.org/10.1002/oby.22831
Sattar N, McInnes IB and McMurray JJ. Obesity is a risk factor for severe COVID-19 infection: multiple potential mechanisms. Circulation. 2020; 142: 4-6. https://doi.org/10.1161/CIRCULATIONAHA.120.047659
Green WD and Beck MA. Obesity Impairs the Adaptive Immune Response to Influenza Virus. Ann Am Thorac Soc. 2017; 14: S406. https://doi.org/10.1513/AnnalsATS.201706-447AW
Leung J, Niikura M, Yang C and Sin D. COVID-19 and COPD. Eur Respir J. 2020; 56. https://doi.org/10.1183/13993003.02108-2020
Yang J, Zheng Y, Gou X, et al. Prevalence of comorbidities in the novel Wuhan coronavirus (COVID-19) infection: a systematic review and meta-analysis. Int J Infect Dis. 2020; 94: 91-5. https://doi.org/10.1016/j.ijid.2020.03.017
Scobey T, Yount B, Sims A, et al. Reverse genetics with a full-length infectious cDNA of the Middle East respiratory syndrome coronavirus. Proc Natl Acad Sci U S A. 2013; 110: 16157-62. https://doi.org/10.1073/pnas.1311542110
Assiri A, Al-Tawfiq J, Al-Rabeeah A, et al. Epidemiological, demographic, and clinical characteristics of 47 cases of Middle East respiratory syndrome coronavirus disease from Saudi Arabia: a descriptive study. Lancet Infect Dis. 2013; 13: 752-61. https://doi.org/10.1016/S1473-3099(13)70204-4
Assiri A, McGeer A, Perl T, et al. Hospital outbreak of Middle East respiratory syndrome coronavirus. N Engl J Med. 2013; 369: 407-16. https://doi.org/10.1056/NEJMoa1306742
Booth C, Matukas L, Tomlinson G, et al. Clinical features and short-term outcomes of 144 patients with SARS in the greater Toronto area. JAMA. 2003; 289: 2801-9. https://doi.org/10.1001/jama.289.21.JOC30885
Robinson D and Klein S. Pregnancy and pregnancy-associated hormones alter immune responses and disease pathogenesis. Horm Behav. 2012; 62: 263-71. https://doi.org/10.1016/j.yhbeh.2012.02.023
Gottfredsson M. The Spanish flu in Iceland 1918. Lessons in medicine and history. Laeknabladid. 2008; 94: 737-45.
Ng W, Wong S, Lam A, et al. The placentas of patients with severe acute respiratory syndrome: a pathophysiological evaluation. Pathol. 2006; 38: 210-8. https://doi.org/10.1080/00313020600696280
Assiri A, Abedi G, Al MM, Bin AS, Gerber S and Watson J. Middle East Respiratory Syndrome Coronavirus Infection During Pregnancy: A Report of 5 Cases From Saudi Arabia. Clin Infect Dis. 2016; 63: 951-3. https://doi.org/10.1093/cid/ciw412
Wong SF, Chow KM, Leung TN, et al. Pregnancy and perinatal outcomes of women with severe acute respiratory syndrome. Am J Obstet Gynecol. 2004; 191: 292-7. https://doi.org/10.1016/j.ajog.2003.11.019
Zhu H, Wang L, Fang C, et al. Clinical analysis of 10 neonates born to mothers with 2019-nCoV pneumonia. Transl Pediatr. 2020; 9: 51-60. https://doi.org/10.21037/tp.2020.02.06
Chen H, Guo J and Wang C. and intrauterine vertical transmission potential of COVID-19 infection in nine pregnant women: a retrospective review of medical records. Lancet 2020; 395: 809-15. 2020. https://doi.org/10.1016/S0140-6736(20)30360-3
Shek C, Ng P, Fung G, et al. Infants born to mothers with severe acute respiratory syndrome. Pediatrics. 2003; 112: e254-e. https://doi.org/10.1542/peds.112.4.e254
Gagneur A, Dirson E, Audebert S, et al. Vertical transmission of human coronavirus. Prospective pilot study. Pathol Biol (Paris). 2007; 55: 525-30. https://doi.org/10.1016/j.patbio.2007.07.013
Lam C, Wong S, Leung T, et al. A case-controlled study comparing clinical course and outcomes of pregnant and non-pregnant women with severe acute respiratory syndrome. BJOG. 2004; 111: 771-4. https://doi.org/10.1111/j.1471-0528.2004.00199.x
Breslin N, Baptiste C, Gyamfi-Bannerman C, et al. COVID-19 infection among asymptomatic and symptomatic pregnant women: Two weeks of confirmed presentations to an affiliated pair of New York City hospitals. Am J Obstet Gynecol. 2020; 2: 100118. https://doi.org/10.1016/j.ajogmf.2020.100118
Capobianco G, Saderi L, Aliberti S, et al. COVID-19 in pregnant women: A systematic review and meta-analysis. Eur J Obstet Gynecol Reprod Biol. 2020; 252: 543-58. https://doi.org/10.1016/j.ejogrb.2020.07.006
Jering KS, Claggett BL, Cunningham JW, et al. Clinical Characteristics and Outcomes of Hospitalized Women Giving Birth With and Without COVID-19. JAMA Internal Medicine.
Alfaraj S, Al-Tawfiq J and Memish Z. Middle East Respiratory Syndrome Coronavirus (MERS-CoV) infection during pregnancy: Report of two cases & review of the literature. J Microbiol Immunol Infect. 2019; 52: 501-3. https://doi.org/10.1016/j.jmii.2018.04.005
Malik A, El KM, Ravi M and Sayed F. Middle East Respiratory Syndrome Coronavirus during Pregnancy, Abu Dhabi, United Arab Emirates, 2013. Emerg Infect Dis. 2016; 22: 515-7. https://doi.org/10.3201/eid2203.151049
Hon K, Leung C, Cheng W, et al. Clinical presentations and outcome of severe acute respiratory syndrome in children. The Lancet. 2003; 361: 1701-3. https://doi.org/10.1016/S0140-6736(03)13364-8
Al-Tawfiq J, Kattan R and Memish Z. Middle East respiratory syndrome coronavirus disease is rare in children: An update from Saudi Arabia. World J Clin Pediatr. 2016; 5: 391-6. https://doi.org/10.5409/wjcp.v5.i4.391
Fagbo S, Garbati M, Hasan R, et al. Acute viral respiratory infections among children in MERS-endemic Riyadh, Saudi Arabia, 2012-2013. J Med Virol. 2017; 89: 195-201. https://doi.org/10.1002/jmv.24632
Kelvin A and Halperin S. COVID-19 in children: the link in the transmission chain. Lancet Infect Dis. 2020; 20: 633-4. https://doi.org/10.1016/S1473-3099(20)30236-X
Wei M, Yuan J, Liu Y, Fu T, Yu X and Zhang Z-J. Novel coronavirus infection in hospitalized infants under 1 year of age in China. Jama. 2020; 323: 1313-4. https://doi.org/10.1001/jama.2020.2131
Li A, So H, Chu W, et al. Radiological and pulmonary function outcomes of children with SARS. Pediatr Pulmonol. 2004; 38: 427-33. https://doi.org/10.1002/ppul.20078
Chan JF-W, Yuan S, Kok K-H, et al. A familial cluster of pneumonia associated with the 2019 novel coronavirus indicating person-to-person transmission: a study of a family cluster. The Lancet. 2020; 395: 514-23. https://doi.org/10.1016/S0140-6736(20)30154-9
Young BE, Ong SWX, Kalimuddin S, et al. Epidemiologic features and clinical course of patients infected with SARS-CoV-2 in Singapore. Jama. 2020; 323: 1488-94. https://doi.org/10.1001/jama.2020.3204
Liu K, Fang Y, Deng Y, et al. Clinical characteristics of novel coronavirus cases in tertiary hospitals in Hubei Province. Chin Med J (Engl). 2020; 133: 1025-31. https://doi.org/10.1097/CM9.0000000000000744
Liu Y, Yang Y, Zhang C, et al. Clinical and biochemical indexes from 2019-nCoV infected patients linked to viral loads and lung injury. Sci China Life Sci. 2020; 63: 364-74. https://doi.org/10.1007/s11427-020-1643-8
Guan W, Ni Z, Hu Y, et al. Clinical Characteristics of Coronavirus Disease 2019 in China. N Engl J Med. 2020; 382: 1708-20. https://doi.org/10.1056/NEJMoa2002032
Published
How to Cite
Issue
Section
Copyright (c) 2021 International Journal of Clinical Research

This work is licensed under a Creative Commons Attribution 4.0 International License.







