Borderline Serous Papillary Tumor Arising in a Paraovarian Cyst: A Case Report and an Extensive Review of the Literature
DOI:
https://doi.org/10.38179/ijcr.v2i1.72Keywords:
Borderline papillary tumor, Papillary projections, Paraovarian cyst, Excision, Case reportAbstract
Background: Paraovarian cysts are benign cysts that develop near the ovaries and fallopian tubes in the pelvic region. They can cause mass effects requiring excision. In rare cases, tumors may develop inside these cysts. These tumors may be benign, malignant, or borderline.
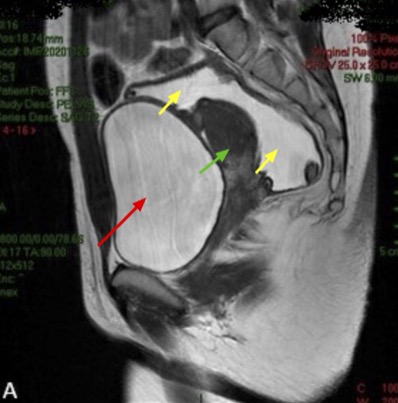
Case Report: A 26-year-old lady presented for excision of a paraovarian cyst. Pre-operative imaging showed the presence of few undulating folds at the periphery of the cyst. The patient underwent laparoscopic pelvic cystectomy without intra-operative drainage. Pathological examination of the specimen revealed a borderline serous papillary tumor protruding from the cyst wall.
Conclusion: The occurrence of a borderline tumor, also known as a tumor of low malignant potential, in a pre-existing paraovarian cyst is very rare and has only been reported few times in the literature. A thorough review of these cases showed that the most common imaging finding that raises suspicion for a borderline tumor within a paraovarian cyst is the presence of small intracystic projections within the unilocular adnexal cyst. However, since evaluating the presence of an intracystic tumor is not always possible, performing a fertility-preserving laparoscopic cystectomy without cyst content spillage, is recommended. If properly excised, the prognosis of this tumor is good, and recurrence is rare.
References
Kiseli M, Caglar GS, Cengiz SD, et al. Clinical diagnosis and complications of paratubal cysts: review of the literature and report of uncommon presentations. Arch Gynecol Obstet. 2012;285(6):1563-1569. PMID: 22526447. https://doi.org/10.1007/s00404-012-2304-8
Kim JS, Woo SK, Suh SJ, Morettin LB. Sonographic diagnosis of paraovarian cysts: value of detecting a separate ipsilateral ovary. AJR Am J Roentgenol. 1995;164(6):1441-1444. PMID: 7754888. https://doi.org/10.2214/ajr.164.6.7754888
Stein AL, Koonings PP, Schlaerth JB, et al. Relative frequency of malignant parovarian tumors: should parovarian tumors be aspirated?. Obstet Gynecol. 1990;75(6):1029-1031. PMID: 2140437.
Salamon C, Tornos C, Chi DS. Borderline endometrioid tumor arising in a paratubal cyst: a case report. Gynecol Oncol. 2005;97(1):263-265. PMID: 15790473. https://doi.org/10.1016/j.ygyno.2004.12.032
Mehawej J, El Helou N, Wang L, Mhawech-Fauceglia P. Paratubal serous borderline tumor in an 85 years old woman: A case report. Gynecol Oncol Rep. 2020;32:100559. PMID: 32258331. https://doi.org/10.1016/j.gore.2020.100559
Moyle PL, Kataoka MY, Nakai A, et al. Nonovarian cystic lesions of the pelvis. Radiographics. 2010;30(4):921-938. PMID: 20631360. https://doi.org/10.1148/rg.304095706
Darwish AM, Amin AF, Mohammad SA. Laparoscopic management of paratubal and paraovarian cysts. JSLS. 2003;7(2):101-106. PMID: 12856838.
Liu C, Wu R, Sun X, Tao C, Liu Z. Risk factors for delayed hemorrhage after colonoscopic postpolypectomy: Polyp size and operative modality. JGH Open. 2018;3(1):61-64. PMID: 30834342. https://doi.org/10.1002/jgh3.12106
Kishimoto K, Ito K, Awaya H, et al. Paraovarian cyst: MR imaging features. Abdom Imaging. 2002;27(6):685-689. PMID: 12395257. https://doi.org/10.1007/s00261-002-0014-6
Durairaj A, Gandhiraman K. Complications and Management of Paraovarian Cyst: A Retrospective Analysis. J Obstet Gynaecol India. 2019;69(2):180-184. PMID: 30956474. https://doi.org/10.1007/s13224-018-1152-2
Lucey BC, Kuligowska E. Radiologic management of cysts in the abdomen and pelvis. AJR Am J Roentgenol. 2006;186(2):562-573. PMID: 16423969. https://doi.org/10.2214/ajr.04.1051
García-Tejedor A, Castellarnau M, Burdio F, et al. Ultrasound-guided aspiration of adnexal cysts with a low risk of malignancy: is it a recommendable option?. J Ultrasound Med. 2015;34(6):985-991. PMID: 26014317. https://doi.org/10.7863/ultra.34.6.985
Levine D, Brown DL, Andreotti RF, et al. Management of asymptomatic ovarian and other adnexal cysts imaged at US Society of Radiologists in Ultrasound consensus conference statement. Ultrasound Q. 2010;26(3):121-131. PMID: 20823748. https://doi.org/10.1097/ruq.0b013e3181f09099
Thakore SS, Chun MJ, Fitzpatrick K. Recurrent ovarian torsion due to paratubal cysts in an adolescent female. J Pediatr Adolesc Gynecol. 2012;25(4):e85-e87. PMID: 22840942. https://doi.org/10.1016/j.jpag.2011.10.012
Kajiyama A, Edo H, Takeya C, et al. Spontaneously Ruptured Paraovarian Tumor of Borderline Malignancy with Extremely Elevated Serum Carbohydrate Antigen 125 (CA125) Levels: A Comparison of the Imaging and Pathological Features. Am J Case Rep. 2017;18:919-925. PMID: 28835604. https://doi.org/10.12659/ajcr.904462
Savelli L, Ghi T, De Iaco P, et al. Paraovarian/paratubal cysts: comparison of transvaginal sonographic and pathological findings to establish diagnostic criteria. Ultrasound Obstet Gynecol. 2006;28(3):330-334. PMID: 16823765. https://doi.org/10.1002/uog.2829
Smorgick N, Herman A, Schneider D, et al. Paraovarian cysts of neoplastic origin are underreported. JSLS. 2009;13(1):22-26. PMID: 19366536.
Scully RE, Bonfiglio TA, Kurman RJ, et al. Histological Typing of Female Genital Tract Tumours. Berlin, Heidelberg: Springer Berlin Heidelberg. 1994. https://doi.org/10.1007/978-3-642-85014-1.
Im HS, Kim JO, Lee SJ, et al. Borderline mucinous tumor arising in a paratubal cyst: a case report. Eur J Gynaecol Oncol. 2011;32(2):206-207. PMID: 21614917.
Chandraratnam E, Leong AS. Papillary serous cystadenoma of borderline malignancy arising in a parovarian paramesonephric cyst. Light microscopic and ultrastructural observations. Histopathology. 1983;7(4):601-611. PMID: 6885002. https://doi.org/10.1111/j.1365-2559.1983.tb02272.x
De Areia AL, Frutuoso C, Amaral N, Dias I, De Oliveira C. Paraovarian tumor of borderline malignancy--a case report. Int J Gynecol Cancer. 2004;14(4):680-682. PMID: 15304166. https://doi.org/10.1111/j.1048-891x.2004.14428.x
Barloon TJ, Brown BP, Abu-Yousef MM, Warnock NG. Paraovarian and paratubal cysts: preoperative diagnosis using transabdominal and transvaginal sonography. J Clin Ultrasound. 1996;24(3):117-122. PMID: 8838299. https://doi.org/10.1002/(sici)1097-0096(199603)24:3%3C117::aid-jcu2%3E3.0.co;2-k
Buamah P. Benign conditions associated with raised serum CA-125 concentration. J Surg Oncol. 2000;75(4):264-265. PMID: 11135268. https://doi.org/10.1002/1096-9098(200012)75:4%3C264::aid-jso7%3E3.0.co;2-q
Montavon Sartorius C, Mirza U, Schötzau A, et al. Impact of the new FIGO 2013 classification on prognosis of stage I epithelial ovarian cancers. Cancer Manag Res. 2018;10:4709-4718. PMID: 30410404. https://doi.org/10.2147/cmar.s174777
Baek J. Paratubal borderline serous tumor in a postmenopausal woman: a case report. Pan Afr Med J. 2019;32:129. PMID: 31223417. https://doi.org/10.11604/pamj.2019.32.129.18031
Seamon LG, Holt CN, Suarez A, et al. Paratubal borderline serous tumors. Gynecol Oncol. 2009;113(1):83-85. PMID: 19189870. https://doi.org/10.1016/j.ygyno.2008.12.019
Terek MC, Sahin C, Yeniel AO, et al. Paratubal borderline tumor diagnosed in the adolescent period: a case report and review of the literature. J Pediatr Adolesc Gynecol. 2011;24(5):e115-e116. PMID: 21737318. https://doi.org/10.1016/j.jpag.2011.05.007
Shin YJ, Kim JY, Lee HJ, et al. Paratubal serous borderline tumor. J Gynecol Oncol. 2011;22(4):295-298. PMID: 22247808. https://doi.org/10.3802/jgo.2011.22.4.295
Kumbak B, Celik H, Cobanoglu B, Gurates B. Paratubal borderline tumor incidentally found during cesarean section: case report and review of literature. Eur J Surg Oncol. 2010;36(8):789-791. PMID: 20609550. https://doi.org/10.1016/j.ejso.2010.06.019
Alaoui FZ, El Fatemi H, Chaara H, et al. Borderline paratubal cyst: a case report. Pan Afr Med J. 2012;13:53. PMID: 23330044.
Suzuki S, Furukawa S, Kyozuka H, et al. Two cases of paraovarian tumor of borderline malignancy. J Obstet Gynaecol Res. 2013;39(1):437-441. PMID: 22889349. https://doi.org/10.1111/j.1447-0756.2012.01953.x
Zhao F, Zhang H, Ren Y, Kong F. Transvaginal sonographic characteristics of paraovarian borderline tumor. Int J Clin Exp Med. 2015;8(2):2684-2688. PMID: 25932220.
Lee S, Ahn KH, Park HT, et al. Paratubal Borderline Malignancy: A Case of a 17-Year-Old Adolescent Female Treated with Laparo-Endoscopic Single-Site Surgery and a Review of the Literature. J Pediatr Adolesc Gynecol. 2016;29(1):74-76. PMID: 26026220. https://doi.org/10.1016/j.jpag.2014.07.012
Chao A, Huang YL, Lin CY, et al. A Case of Paratubal Serous Borderline Tumor Driven by a Somatic BRAF Mutation in an Adolescent Patient. J Pediatr Adolesc Gynecol. 2021;34(2):228-230. PMID: 33188936. https://doi.org/10.1016/j.jpag.2020.11.008
Published
How to Cite
Issue
Section
Copyright (c) 2021 International Journal of Clinical Research

This work is licensed under a Creative Commons Attribution 4.0 International License.







